The Ocular Surface ( IF 6.4 ) Pub Date : 2023-09-25 , DOI: 10.1016/j.jtos.2023.09.008 Mohammad Soleimani 1 , Reza Mirshahi 2 , Kasra Cheraqpour 3 , Seyed Mahbod Baharnoori 4 , Hamed Massoumi 4 , Collin Chow 5 , Sumaiya Shahjahan 6 , Bita Momenaei 7 , Mohammad Javad Ashraf 4 , Raghuram Koganti 4 , Mahmood Ghassemi 4 , Khandaker N Anwar 4 , Elmira Jalilian 4 , Ali R Djalilian 4
|
Purpose
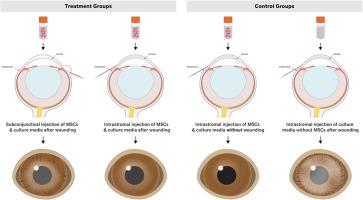
Different approaches to delivery of mesenchymal stem/stromal cells (MSCs) for ameliorating corneal injuries have been investigated. This study was aimed to compare the efficacy of intrastromal and subconjunctival injection of human bone marrow-derived MSCs (hBM-MSCs) in a corneal epithelial injury model.
Methods
Twenty-four C57BL/6J mice underwent total corneal and limbal epithelial debridement. Then, the mice were divided into three different groups: (1) intrastromal hBM-MSCs injection, (2) subconjunctival hBM-MSCs injection, and (3) injection of frozen medium as a control. Mice were monitored by slit lamp and underwent anterior segment optical coherence tomography (ASOCT). Following euthanasia, the corneas were further evaluated by histology and immunostaining.
Results
hBM-MSC injection successfully healed epithelial defects regardless of the delivery route (P < 0.001). However, intrastromal injection was superior to subconjunctival injection in reducing defect area (P = 0.001). Intrastromal injection of hBM-MSCs also significantly reduced corneal opacity and neovascularization and improved ASOCT parameters compared to subconjunctival injection or no treatment (P < 0.001, P = 0.003, and P < 0.001, respectively). Although both of the treatment groups were positive for CK12 and had reduced levels of MUC5AC compared to the control, CK12 staining was stronger in the intrastromal group compared to the subconjunctival group. Also, persistency of MSCs was confirmed by in vivo (up to 2 weeks) and in vitro assessments (up to 4 weeks).
Conclusions
Although the injection of hBM-MSC using both intrastromal and subconjunctival methods improve wound healing and reduce neovascularization and opacity, the intrastromal approach is superior in terms of corneal healing.
中文翻译:

基质内与结膜下注射间充质干细胞/基质细胞促进角膜修复
目的
已经研究了用于改善角膜损伤的间充质干细胞/基质细胞(MSC)的不同递送方法。本研究旨在比较在角膜上皮损伤模型中基质内和结膜下注射人骨髓源性间充质干细胞(hBM-MSCs)的效果。
方法
24 只 C57BL/6J 小鼠接受了全角膜和角膜缘上皮清创术。然后,将小鼠分为三个不同组:(1)基质内hBM-MSCs注射,(2)结膜下hBM-MSCs注射,和(3)注射冷冻培养基作为对照。通过裂隙灯监测小鼠并进行眼前节光学相干断层扫描(ASOCT)。安乐死后,通过组织学和免疫染色进一步评估角膜。
结果
无论输送途径如何, hBM-MSC 注射都能成功治愈上皮缺损(P < 0.001)。然而,在减少缺损面积方面,基质内注射优于结膜下注射(P = 0.001)。与结膜下注射或不治疗相比,基质内注射 hBM-MSC 还显着降低了角膜混浊和新生血管形成,并改善了 ASOCT 参数(分别为 P < 0.001、P = 0.003 和 P < 0.001)。尽管两个治疗组的 CK12 均为阳性,并且与对照组相比,MUC5AC 水平降低,但基质内组的 CK12 染色强于结膜下组。此外,MSC 的持久性通过体内(长达 2 周)和体外评估(长达 4 周)得到证实。
结论
尽管使用基质内和结膜下方法注射hBM-MSC可以改善伤口愈合并减少新生血管形成和混浊,但基质内方法在角膜愈合方面更优越。
































 京公网安备 11010802027423号
京公网安备 11010802027423号