Abstract
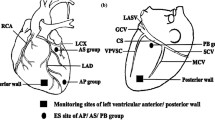
Cardiac sympathetic overactivation is a critical driver in the progression of acute myocardial infarction (AMI). The left middle cervical ganglion (LMCG) is an important extracardiac sympathetic ganglion. However, the regulatory effects of LMCG on AMI have not yet been fully documented. In the present study, we detected that the LMCG was innervated by abundant sympathetic components and exerted an excitatory effect on the cardiac sympathetic nervous system in response to stimulation. In canine models of AMI, targeted ablation of LMCG reduced the sympathetic indexes of heart rate variability and serum norepinephrine, resulting in suppressed cardiac sympathetic activity. Moreover, LMCG ablation could improve ventricular electrophysiological stability, evidenced by the prolonged ventricular effective refractory period, elevated action potential duration, increased ventricular fibrillation threshold, and enhanced connexin43 expression, consequently showing antiarrhythmic effects. Additionally, compared with the control group, myocardial infarction size, circulating cardiac troponin I, and myocardial apoptosis were significantly reduced, accompanied by preserved cardiac function in canines subjected to LMCG ablation. Finally, we performed the left stellate ganglion (LSG) ablation and compared its effects with LMCG destruction. The results indicated that LMCG ablation prevented ventricular electrophysiological instability, cardiac sympathetic activation, and AMI-induced ventricular arrhythmias with similar efficiency as LSG denervation. In conclusion, this study demonstrated that LMCG ablation suppressed cardiac sympathetic activity, stabilized ventricular electrophysiological properties and mitigated cardiomyocyte death, resultantly preventing ischemia-induced ventricular arrhythmias, myocardial injury, and cardiac dysfunction. Neuromodulation therapy targeting LMCG represented a promising strategy for the treatment of AMI.










Similar content being viewed by others
Data availability
The datasets are available on reasonable request to the corresponding author.
References
Abumandour MMA, Hanafy BG, Morsy K, El-Kott A, Shati A, Salah El-Din E, Bassuoni NF (2022) Cervicothoracic sympathetic system in the dog: new insights by the gross morphological description of each ganglion with its branches on each side. Folia Morphol (Warsz) 81:20–30. https://doi.org/10.5603/FM.a2021.0009
Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB, Deal BJ, Dickfeld T, Field ME, Fonarow GC, Gillis AM, Granger CB, Hammill SC, Hlatky MA, Joglar JA, Kay GN, Matlock DD, Myerburg RJ, Page RL (2018) 2017 AHA/ACC/HRS Guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: executive summary: a report of the American college of cardiology/American heart association task force on clinical practice guidelines and the heart rhythm society. Circulation 138:e210–e271. https://doi.org/10.1161/cir.0000000000000548
Albani S, Fabris E, Doimo S, Barbati G, Perkan A, Merlo M, Gatti G, Di Lenarda A, Van’t Hof AWJ, Maras P, Sinagra G (2018) Early occurrence of drug intolerance as risk factor during follow-up in patients with acute coronary syndrome or coronary revascularization. Eur Heart J Cardiovasc Pharmacother 4:195–201. https://doi.org/10.1093/ehjcvp/pvy017
Ali R, Ciccone J, Tseng V (2017) Cervical sympathetic blockade for the management of electrical storm. J Clin Anesth 36:47–50. https://doi.org/10.1016/j.jclinane.2016.07.037
Amgalan D, Pekson R, Kitsis RN (2017) Troponin release following brief myocardial ischemia: apoptosis versus necrosis. JACC Basic Transl Sci 2:118–121. https://doi.org/10.1016/j.jacbts.2017.03.008
Del Re DP, Amgalan D, Linkermann A, Liu Q, Kitsis RN (2019) Fundamental mechanisms of regulated cell death and implications for heart disease. Physiol Rev 99:1765–1817. https://doi.org/10.1152/physrev.00022.2018
Forrester SJ, Booz GW, Sigmund CD, Coffman TM, Kawai T, Rizzo V, Scalia R, Eguchi S (2018) Angiotensin II signal transduction: an update on mechanisms of physiology and pathophysiology. Physiol Rev 98:1627–1738. https://doi.org/10.1152/physrev.00038.2017
Frangogiannis NG (2015) Pathophysiology of Myocardial Infarction. Compr Physiol 5:1841–1875. https://doi.org/10.1002/cphy.c150006
Goldberger JJ, Arora R, Buckley U, Shivkumar K (2019) Autonomic nervous system dysfunction: JACC focus seminar. J Am Coll Cardiol 73:1189–1206. https://doi.org/10.1016/j.jacc.2018.12.064
Herring N, Kalla M, Paterson DJ (2019) The autonomic nervous system and cardiac arrhythmias: current concepts and emerging therapies. Nat Rev Cardiol 16:707–726. https://doi.org/10.1038/s41569-019-0221-2
Heusch G (1990) Alpha-adrenergic mechanisms in myocardial ischemia. Circulation 81:1–13. https://doi.org/10.1161/01.cir.81.1.1
Heusch G, Baumgart D, Camici P, Chilian W, Gregorini L, Hess O, Indolfi C, Rimoldi O (2000) alpha-adrenergic coronary vasoconstriction and myocardial ischemia in humans. Circulation 101:689–694. https://doi.org/10.1161/01.cir.101.6.689
Heusch G, Deussen A, Thamer V (1985) Cardiac sympathetic nerve activity and progressive vasoconstriction distal to coronary stenoses: feed-back aggravation of myocardial ischemia. J Auton Nerv Syst 13:311–326. https://doi.org/10.1016/0165-1838(85)90020-7
Hopf HB, Skyschally A, Heusch G, Peters J (1995) Low-frequency spectral power of heart rate variability is not a specific marker of cardiac sympathetic modulation. Anesthesiology 82:609–619. https://doi.org/10.1097/00000542-199503000-00002
Irie T, Yamakawa K, Hamon D, Nakamura K, Shivkumar K, Vaseghi M (2017) Cardiac sympathetic innervation via middle cervical and stellate ganglia and antiarrhythmic mechanism of bilateral stellectomy. Am J Physiol Heart Circ Physiol 312:H392–H405. https://doi.org/10.1152/ajpheart.00644.2016
Jia XF, Liang FG, Kitsis RN (2021) Multiple Cell Death Programs Contribute to Myocardial Infarction. Circ Res 129:397–399. https://doi.org/10.1161/CIRCRESAHA.121.319584
Kawashima T (2005) The autonomic nervous system of the human heart with special reference to its origin, course, and peripheral distribution. Anat Embryol (Berl) 209:425–438. https://doi.org/10.1007/s00429-005-0462-1
Kokubun S, Sato T, Yajima T, Ichikawa H (2019) Distribution of postganglionic neurons which contain dopamine beta-hydroxylase, tyrosine hydroxylase, neuropeptide Y and vasoactive intestinal polypeptide in the human middle cervical ganglion. Tissue Cell 58:42–50. https://doi.org/10.1016/j.tice.2019.04.006
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 16:233–270. https://doi.org/10.1093/ehjci/jev014
Liu S, Yu X, Luo D, Qin Z, Wang X, He W, Ma R, Hu H, Xie J, He B, Lu Z, Jiang H (2018) Ablation of the ligament of marshall and left stellate ganglion similarly reduces ventricular arrhythmias during acute myocardial infarction. Circ Arrhythm Electrophysiol 11:e005945. https://doi.org/10.1161/CIRCEP.117.005945
Manolis AA, Manolis TA, Apostolopoulos EJ, Apostolaki NE, Melita H, Manolis AS (2021) The role of the autonomic nervous system in cardiac arrhythmias: the neuro-cardiac axis, more foe than friend? Trends Cardiovasc Med 31:290–302. https://doi.org/10.1016/j.tcm.2020.04.011
Markman TM, Gugger D, Arkles J, Riley MP, Dixit S, Guandalini GS, Frankel DS, Epstein AE, Callans DJ, Singhal S, Marchlinski FE, Nazarian S (2023) Neuromodulation for the treatment of refractory ventricular arrhythmias. JACC Clin Electrophysiol 9:161–169. https://doi.org/10.1016/j.jacep.2022.08.031
Meng L, Tseng CH, Shivkumar K, Ajijola O (2017) Efficacy of Stellate ganglion blockade in managing electrical storm: a systematic review. JACC Clin Electrophysiol 3:942–949. https://doi.org/10.1016/j.jacep.2017.06.006
Okninska M, Maczewski M, Mackiewicz U (2022) Ventricular arrhythmias in acute myocardial ischaemia-Focus on the ageing and sex. Ageing Res Rev 81:101722. https://doi.org/10.1016/j.arr.2022.101722
Ouwerkerk W, Voors AA, Anker SD, Cleland JG, Dickstein K, Filippatos G, van der Harst P, Hillege HL, Lang CC, Ter Maaten JM, Ng LL, Ponikowski P, Samani NJ, van Veldhuisen DJ, Zannad F, Metra M, Zwinderman AH (2017) Determinants and clinical outcome of uptitration of ACE-inhibitors and beta-blockers in patients with heart failure: a prospective European study. Eur Heart J 38:1883–1890. https://doi.org/10.1093/eurheartj/ehx026
Papa A, Kushner J, Marx SO (2022) Adrenergic Regulation of Calcium Channels in the Heart. Annu Rev Physiol 84:285–306. https://doi.org/10.1146/annurev-physiol-060121-041653
Rodriguez-Sinovas A, Sanchez JA, Valls-Lacalle L, Consegal M, Ferreira-Gonzalez I (2021) Connexins in the Heart: Regulation, Function and Involvement in Cardiac Disease. Int J Mol Sci 22:4413. https://doi.org/10.3390/ijms22094413
Ruiz-Meana M, Rodríguez-Sinovas A, Cabestrero A, Boengler K, Heusch G, Garcia-Dorado D (2008) Mitochondrial connexin43 as a new player in the pathophysiology of myocardial ischaemia-reperfusion injury. Cardiovasc Res 77:325–333. https://doi.org/10.1093/cvr/cvm062
Schwartz PJ, Ackerman MJ (2022) Cardiac sympathetic denervation in the prevention of genetically mediated life-threatening ventricular arrhythmias. Eur Heart J 43:2096–2102. https://doi.org/10.1093/eurheartj/ehac134
Shivkumar K, Ajijola OA, Anand I, Armour JA, Chen PS, Esler M, De Ferrari GM, Fishbein MC, Goldberger JJ, Harper RM, Joyner MJ, Khalsa SS, Kumar R, Lane R, Mahajan A, Po S, Schwartz PJ, Somers VK, Valderrabano M, Vaseghi M, Zipes DP (2016) Clinical neurocardiology defining the value of neuroscience-based cardiovascular therapeutics. J Physiol 594:3911–3954. https://doi.org/10.1113/jp271870
Singh K, Communal C, Sawyer DB, Colucci WS (2000) Adrenergic regulation of myocardial apoptosis. Cardiovasc Res 45:713–719. https://doi.org/10.1016/s0008-6363(99)00370-3
Sorbets E, Steg PG, Young R, Danchin N, Greenlaw N, Ford I, Tendera M, Ferrari R, Merkely B, Parkhomenko A, Reid C, Tardif JC, Fox KM (2019) β-blockers, calcium antagonists, and mortality in stable coronary artery disease: an international cohort study. Eur Heart J 40:1399–1407. https://doi.org/10.1093/eurheartj/ehy811
Van Weperen VYH, Vos MA, Ajijola OA (2021) Autonomic modulation of ventricular electrical activity: recent developments and clinical implications. Clin Auton Res 31:659–676. https://doi.org/10.1007/s10286-021-00823-4
Vaseghi M, Barwad P, Malavassi Corrales FJ, Tandri H, Mathuria N, Shah R, Sorg JM, Gima J, Mandal K, Saenz Morales LC, Lokhandwala Y, Shivkumar K (2017) Cardiac sympathetic denervation for refractory ventricular arrhythmias. J Am Coll Cardiol 69:3070–3080. https://doi.org/10.1016/j.jacc.2017.04.035
Yoshie K, Rajendran PS, Massoud L, Mistry J, Swid MA, Wu X, Sallam T, Zhang R, Goldhaber JI, Salavatian S, Ajijola OA (2020) Cardiac TRPV1 afferent signaling promotes arrhythmogenic ventricular remodeling after myocardial infarction. JCI Insight 5:e124477. https://doi.org/10.1172/jci.insight.124477
Yu L, Zhou L, Cao G, Po SS, Huang B, Zhou X, Wang M, Yuan S, Wang Z, Wang S, Jiang H (2017) Optogenetic modulation of cardiac sympathetic nerve activity to prevent ventricular arrhythmias. J Am Coll Cardiol 70:2778–2790. https://doi.org/10.1016/j.jacc.2017.09.1107
Yu X, He W, Xie J, He B, Luo D, Wang X, Jiang H, Lu Z (2019) Selective ablation of ligament of Marshall inhibits ventricular arrhythmias during acute myocardial infarction: possible mechanisms. J Cardiovasc Electrophysiol 30:374–382. https://doi.org/10.1111/jce.13802
Zhang S, Wang M, Jiao L, Liu C, Chen H, Zhou L, Wang Y, Wang Y, Liu Z, Liu Z, Zhou Y, Zhou H, Xu X, Li Z, Liu Z, Yu Z, Nie L, Yu L, Jiang H (2022) Ultrasound-guided injection of botulinum toxin type A blocks cardiac sympathetic ganglion to improve cardiac remodeling in a large animal model of chronic myocardial infarction. Heart Rhythm 19:2095–2104. https://doi.org/10.1016/j.hrthm.2022.08.002
Zhou Z, Liu C, Xu S, Wang J, Guo F, Duan S, Deng Q, Sun J, Yu F, Zhou Y, Wang M, Wang Y, Zhou L, Jiang H, Yu L (2022) Metabolism regulator adiponectin prevents cardiac remodeling and ventricular arrhythmias via sympathetic modulation in a myocardial infarction model. Basic Res Cardiol 117:34. https://doi.org/10.1007/s00395-022-00939-2
Acknowledgements
We would like to acknowledge Tuantuan Tan, Yan-hong Tang and Xi Wang for their kind support. We thank Figdraw for providing scientific drawing materials.
Funding
This work was supported by the National Natural Science Foundation of China (82070425 and 82270402 to Zhibing Lu, 82000386 to Ke-Qiong Deng, 82100403 to Chen-Ze Li, and 81900455 to Xiaomei Yu).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing financial interests.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zheng, M., Chen, S., Zeng, Z. et al. Targeted ablation of the left middle cervical ganglion prevents ventricular arrhythmias and cardiac injury induced by AMI. Basic Res Cardiol 119, 57–74 (2024). https://doi.org/10.1007/s00395-023-01026-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00395-023-01026-w