Abstract
Aims/hypothesis
Adults with type 1 diabetes should perform daily physical activity to help maintain health and fitness, but the influence of daily step counts on continuous glucose monitoring (CGM) metrics are unclear. This analysis used the Type 1 Diabetes Exercise Initiative (T1DEXI) dataset to investigate the effect of daily step count on CGM-based metrics.
Methods
In a 4 week free-living observational study of adults with type 1 diabetes, with available CGM and step count data, we categorised participants into three groups—below (<7000), meeting (7000–10,000) or exceeding (>10,000) the daily step count goal—to determine if step count category influenced CGM metrics, including per cent time in range (TIR: 3.9–10.0 mmol/l), time below range (TBR: <3.9 mmol/l) and time above range (TAR: >10.0 mmol/l).
Results
A total of 464 adults with type 1 diabetes (mean±SD age 37±14 years; HbA1c 48.8±8.1 mmol/mol [6.6±0.7%]; 73% female; 45% hybrid closed-loop system, 38% standard insulin pump, 17% multiple daily insulin injections) were included in the study. Between-participant analyses showed that individuals who exceeded the mean daily step count goal over the 4 week period had a similar TIR (75±14%) to those meeting (74±14%) or below (75±16%) the step count goal (p>0.05). In the within-participant comparisons, TIR was higher on days when the step count goal was exceeded or met (both 75±15%) than on days below the step count goal (73±16%; both p<0.001). The TBR was also higher when individuals exceeded the step count goals (3.1%±3.2%) than on days when they met or were below step count goals (difference in means −0.3% [p=0.006] and −0.4% [p=0.001], respectively). The total daily insulin dose was lower on days when step count goals were exceeded (0.52±0.18 U/kg; p<0.001) or were met (0.53±0.18 U/kg; p<0.001) than on days when step counts were below the current recommendation (0.55±0.18 U/kg). Step count had a larger effect on CGM-based metrics in participants with a baseline HbA1c ≥53 mmol/mol (≥7.0%).
Conclusions/interpretation
Our results suggest that, compared with days with low step counts, days with higher step counts are associated with slight increases in both TIR and TBR, along with small reductions in total daily insulin requirements, in adults living with type 1 diabetes.
Data availability
The data that support the findings reported here are available on the Vivli Platform (ID: T1-DEXI; https://doi.org/10.25934/PR00008428).
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Achieving the guidelines of 150 minutes of moderate to vigorous physical activity per week is associated with maintenance of whole-body insulin sensitivity, lower total daily insulin needs, improved cardiovascular health and weight maintenance in adults with type 1 diabetes [1,2,3,4]. While lower mean glucose levels and increased time in range (TIR; glucose level 3.9–10.0 mmol/l) have been reported on days when individuals engage in structured exercise [5, 6], the impact of regular and daily step counts on mean, or 24 h, TIR metrics in type 1 diabetes is unclear.
In addition to structured exercise sessions, which are typically performed for the purpose of improving or maintaining fitness and health, physical activities not typically considered to be exercise per se, such as completing household chores, gardening or walking, can help individuals reach their daily (or weekly) physical activity goals [7]. Wearable fitness monitors, such as smart watches, allow individuals to track both planned and unplanned activity and achievement of physical activity goals by estimating the number of active minutes per week or by counting daily steps using accelerometery [8, 9]. The American College of Sports Medicine recommends that all adults should aim for at least 7000–10,000 (7–10K) steps/day [9], and research demonstrates that ~7–10K steps/day, or more, is associated with a lower risk of all-cause mortality in adults with prediabetes and type 2 diabetes [10]. In 90 children with type 1 diabetes, higher mean step counts were associated with lower blood pressure and a reduction in triglyceride levels, but the effect on interstitial glucose, as measured by continuous glucose monitoring (CGM), was not reported [11].
While a high step count may be associated with health and fitness benefits for people with type 1 diabetes [12], it is currently unclear if elevated step counts are associated with alterations in CGM-based metrics, which encompasses mean glucose, TIR, time above range (TAR; glucose level >10.0 mmol/l) and time below range (TBR; glucose level <3.9 mmol/l) over a given period. Unstructured physical activity is often highly variable between days in adults with type 1 diabetes, which may impact 24 h CGM values. One recent observational post hoc analysis of 18 adults with type 1 diabetes on multiple daily insulin injections (MDI) reported significant associations between daily step counts and mean interstitial glucose level (measured by accelerometery and a blinded CGM, respectively) over a 6-day wear time [13]. However, higher step count days were also associated with higher glucose variability and a higher relative risk for hypoglycaemia both during the day and at night [13]. Moreover, interstitial glucose TIR metrics were not reported.
In this study, we explored the potential relationships between step count and CGM-based metrics in adults with type 1 diabetes using cross-sectional and within-participant analyses of the Type 1 Diabetes Initiative (T1DEXI) dataset.
Methods
Study design
The T1DEXI study cohort, study design, inclusion and exclusion criteria, and methods used have been previously published [14]. In brief, eligible participants aged 18–70 years with a clinical diagnosis of type 1 diabetes of at least 2 years’ duration and a willingness to adhere to the study protocol, which included a minimum exercise goal of 150 min per week, inclusive of their assigned 30 min video-guided exercise sessions, to be performed 2 days per week (aerobic, resistance or interval exercise), were recruited from November 2019 to June 2021.
Participants reported demographics, diabetes history and physical activity patterns through online questionnaires and shared their Dexcom G6 CGM data. Participants used a Verily Study Watch (South San Francisco, CA, USA) to collect heart rate and step count data. Total daily step counts as measured by a wrist-worn activity tracker encompass planned (i.e. jogging, workouts) and unplanned (i.e. climbing stairs, incidental walking with chores) activities (not just walking) and can be used as a reasonable proxy for total daily activity, but they have various sources of error when used in free-living environments [15]. Participants used the T1DEXI cloud-connected smartphone application to report physical activity and food intake behaviours. Insulin metrics for participants using standard insulin pumps or hybrid closed-loop (HCL) systems were downloaded directly from the pumps.
Data and participant inclusion
Data from T1DEXI study participants were assessed at day level, defined as being from 00:00 to 23:59. An analysis day required ≥18 h of activity monitoring (step count) data and ≥18 h of CGM data. Participants’ daily step count was measured by taking the mean daily step count for each qualifying 24 h period identified in the 4 week study period. Using the American College of Sports Medicine’s step count recommendations [8, 9], the step counts on each day and participants’ daily step counts were categorised as below (<7K), meeting (7–10K) or exceeding (>10K) the recommended steps/day. To determine the influence of step count on glycaemic metrics, we examined between-participant (i.e. across the cohort) and within-participant (i.e. day-level) data.
The between-participant analysis provided an opportunity to examine the effects of mean daily step count on various CGM-based metrics over the 4 week time frame at cohort level. To be included in the between-participant analyses, participants needed at least 7 qualifying days (see above).
The within-participant day-level analysis was used to determine the impact of higher step count days on 24 h CGM-based metrics compared with lower step count days. This type of analysis allowed for the removal of several potential participant-specific covariates that might impact the step count and TIR relationship, such as baseline HbA1c level, BMI, age, sex and insulin modality. To be included in the within-participant analysis, participants needed at least 2 qualifying days for each of the three step count categories (<7K, 7–10K and 10K), along with sufficient CGM and activity monitor data for each step count subgroup. A within-participant analysis was also performed by insulin modality and baseline HbA1c.
Statistical analyses and outcomes
The following CGM-based metrics were assessed, with all values expressed as percentages: (1) TIR (3.9–10.0 mmol/l), (2) TAR (>10.0 mmol/l), (3) time >13.9 mmol/l, (4) TBR (<3.9 mmol/l) and (5) time <3.0 mmol/l. For the between-participant analysis, CGM-based outcomes were averaged per participant across the 4 week study period. For the within-participant analysis, CGM-based outcomes were calculated each day and averaged across the step count categories.
Insulin use, macronutrient data, 24 h heart rate data and activity metrics were assessed at day level for both between- and within-participant analyses. To calculate the total daily insulin dose, days with ≥18 h of insulin data were included for participants using a standard insulin pump or HCL system, while all days with a basal and a bolus dose were included for MDI users. A participant’s peak heart rate in beats per minute (bpm) across the entire day, obtained via the study wearable, was used as an indicator of daily exercise intensity. Full 24 h heart rate readings were less common than CGM readings, so days with ≥10 h of heart rate data were used to calculate heart rate metrics. Minutes of exercise per day and carbohydrates consumed per day were taken from self-reported data for days analysed.
Statistical analyses were performed using SAS software version 9.4 (SAS Institute, Cary, NC, USA) and R software version 4.3.1 (R Core Team, Vienna, Austria). For skewed outcomes, means and SDs were calculated using an M-estimator from a robust regression. P values, 95% CIs and adjusted differences between the three step count categories were calculated for CGM-based metrics, insulin, heart rate, meal and exercise outcomes for between-participant and within-participant analyses. Tests were performed pairwise, and multiple comparisons were corrected using the two-stage false-discovery rate correction procedure.
For the between-participant analysis, once individuals were grouped into those below, meeting or exceeding daily step count goals, a linear mixed-effects model adjusting for HbA1c, BMI, age, sex, diabetes duration and insulin modality was used to determine differences in CGM-based metrics and other outcomes between the participant subgroups. For the within-participant analysis, a paired t test was used to determine differences in outcomes for each participant using the three step count categories. If the residuals were skewed, a robust regression model was used instead. Differences in CGM-based metrics among groups are expressed as absolute differences (i.e. % is equivalent to percentage point).
Results
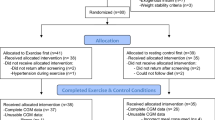
A total of 561 adults were enrolled into the T1DEXI study, with 489 having ≥18 h of CGM data and ≥18 h of step count data per day across 10,316 total days. Figure 1 presents a flow diagram of participant inclusion.
Between-participant analysis
Participant characteristics
The between-participant analysis included 464 participants. Table 1 reports the anthropometric and diabetes-specific characteristics of participants. Participants had a median of 27 days of CGM use and 16 days of study watch use across the 4 week study period. The mean age of participants was 37±14 years, 73% were female and mean BMI was 25.4±4.1 kg/m2. Mean diabetes duration was 18±13 years, and mean baseline HbA1c was 48.8±8.1 mmol/mol (6.6±0.7%). With regard to insulin modality at enrolment, 17% of participants used MDI, 38% used a standard insulin pump and 45% used an HCL system.
CGM-based metrics
The mean TIR was 75% for participants who averaged <7K steps/day (i.e. ‘below’ category), 74% for participants who averaged 7–10K steps/day (i.e. ‘meeting’ category) and 75% for participants who averaged >10K steps/day (i.e. ‘exceeding’ category), with no significant differences after adjusting for baseline HbA1c, BMI, age, sex, diabetes duration and insulin modality (Table 2). Compared with those exceeding the daily step count goal, the mean TBR and time <3.0 mmol/l were slightly lower for participants meeting the daily step count goal (adjusted difference in mean TBR: −1.0% [p=0.001]; <3.0 mmol/l: −0.2% [p=0.02]) and those below the daily step count goal (adjusted difference: −1.3% [p<0.001] and −0.3% [p<0.001], respectively).
Activity data
Compared with a mean maximum daily heart rate of 156 bpm for participants exceeding the daily step count goal, the maximum heart rate was 6 bpm lower for those meeting the daily step count goal (p<0.001) and 8 bpm lower for those below the daily step count goal (p<0.001) after covariate adjustment (Table 2). The mean duration of exercise was 16 min/day lower for those meeting the daily step count goal (p<0.001) and 20 min/day lower for those below the daily step count goal (p<0.001) than the mean duration for those exceeding the daily step count goal (61 min/day) after covariate adjustment.
Meals and insulin metrics
Mean carbohydrate intake and mean total daily insulin dose were similar across the three step count subgroups (Table 2). Mean carbohydrate intake ranged from 132 to 137 g/day across step count groups. The mean total daily insulin dose was 0.57 U/kg for those below the daily step count goal, 0.55 U/kg for those meeting the daily step count goal and 0.50 U/kg for those exceeding the daily step count goal.
Within-participant analysis
CGM-based metrics
The within-participant analyses included 260 participants. Table 3 presents the within-participant outcomes. The mean TIR was higher on days when participants exceeded or met the step count goal (both 75±15%) than on days when the step count was below the step count goal (73±16%; both p<0.001). The mean TAR was lower (p<0.001) on days exceeding or meeting the step count goal (both 21±15%) than on days below the step count goal (24±16%). Compared with days exceeding the step count goal, the mean TBR was slightly lower on days meeting the step count goal (difference: −0.3% [p=0.006]) and on days when it was below the step count goal (adjusted difference: −0.4% [p=0.001]).
Activity data
The within-participant analysis demonstrated that maximum heart rate and exercise duration differed across the step count groups (Table 3). Compared with days exceeding the step count goal, with a mean maximum heart rate of 158 bpm, the mean maximum heart rate was 6 bpm lower for days not meeting the step count goal (p<0.001) and 12 bpm lower for days below the step count goal (p<0.001). Duration of exercise was 45 min lower on days below the step count goal (p<0.001) and 28 min lower on days meeting the step count goal (p<0.001) than on days exceeding the step count goal, for which the mean exercise duration was 72 min/day.
Insulin metrics
Compared with days below the step count goal (0.55±0.18 U/kg), the mean total daily insulin dose across all users was significantly lower on days when the step count goal was met (0.53±0.18 U/kg; p<0.001) or exceeded (0.52±0.18 U/kg; p<0.001) (Table 3).
CGM-based and insulin metrics by insulin modality
When CGM-based metrics were examined by insulin modality (Fig. 2, Table 4), a similar pattern emerged in which mean TIR was slightly higher and mean TAR and time >13.9 mmol/l were slightly lower on days when participants met or exceeded step count goals than on days below the step count goals. Across all insulin modalities, the TBR was slightly elevated when participants were exceeding compared with when they were meeting the daily step count goal (difference in mean TBR for MDI: −0.3% [p=0.03]; standard insulin pump: −0.3% [p=0.008]; HCL: −0.3% [p=0.01]) or when they were below the daily step count goal (MDI: −0.4% [p=0.01]; standard insulin pump: −0.4% [p=0.003]; HCL: −0.04% [p=0.003]). Compared with days meeting the step count goal, exceeding the step count goal increased the mean time <3.0 mmol/l (difference in mean time <3.0 mmol/l for MDI: −0.1% [p=0.14]); standard insulin pump: −0.1% [p=0.04]; HCL: −0.1% [p=0.04]). The p values differed for the various CGM-based metrics across the three insulin modalities, and the relationships between step count category and CGM-based metrics were not entirely duplicated, which may be due to sample size differences. In those using a standard insulin pump or HCL system, the total daily insulin dose was lowest on days when the daily step count goal was exceeded and highest when daily steps were not met. However, this relationship was not observed in MDI users, for whom total daily insulin dose was not associated with daily step count (Table 4).
Box plots showing the relationships between within-participant mean daily step count and TIR metrics according to insulin modality. (a) Per cent TIR: 3.9–10.0 mmol/l; (b) per cent TBR: <3.9 mmol/l; (c) per cent TAR: >10.0 mmol/l. Box plots extend from the 25th to the 75th percentile and whiskers extend from the 10th to the 90th percentiles, horizontal lines within the boxes depict the median and circles depict the mean. *p<0.05, **p<0.01, ***p<0.001 determined from paired t tests or robust regression
CGM-based and insulin metrics by baseline HbA1c
Step count appeared to have a more meaningful effect on CGM-based metrics for individuals with a higher baseline HbA1c (Table 5). For individuals with a higher baseline HbA1c (≥53 mmol/mol [≥7.0%]), mean glucose was lower on days meeting (8.9±1.2 mmol/l) or exceeding (8.9±1.4 mmol/l) the daily step count goal than on days with a lower step count (9.2±1.6 mmol/l; both p=0.001). For individuals with a lower baseline HbA1c (<45 mmol/mol [<6.3%]), all CGM-based metrics were similar by step count group except for TBR. This metric of hypoglycaemia was higher on days exceeding the step count goal (3.9±3.9%) than on days meeting (3.4±3.3%) or below (3.6±3.6%) the step count goal.
Discussion
This study explored the potential associations between mean daily step count and CGM-based metrics in the T1DEXI cohort using between- and within-participant analyses. Based on the between-participant analysis, regularly exceeding 7–10K steps/day does not appear to improve overall TIR significantly in individuals with type 1 diabetes who are already achieving glucose targets (as measured by either TIR or HbA1c levels), and increases TBR slightly, at least compared with averaging <7K steps/day. In contrast, at the within-participant day level, high step count days (>10K) only marginally increase 24 h TIR (by ~2%) relative to low step count days (<7K), and increase TBR (by ~0.4%), even in those using an HCL system. Thus, increasing daily steps does not appear to acutely improve CGM-based metrics in already active adults with type 1 diabetes who are exceeding the consensus-based targets [16].
While higher total physical activity levels do not appear to improve CGM-based metrics in this cohort of adults with type 1 diabetes who are generally achieving glucose targets, we did note other interesting associations. Individuals with the highest mean daily step counts (>10K) had the lowest mean glucose levels, the lowest BMI, the highest daily heart rate, more dedicated physical activity time and the lowest daily insulin dose. Thus, it appears that averaging high step counts may be associated with favourable changes to several physiological metrics. It is also important to acknowledge that, based on other cross-sectional [17, 18] and longitudinal [19] data, higher levels of physical activity appear to promote major improvements in cardiorespiratory fitness, vascular health, skeletal muscle strength and sleep patterns and are associated with reduced all-cause mortality in type 1 diabetes (see [3] for a review). Moreover, undertaking dedicated and structured sessions of aerobic or resistance exercise training over a sustained period (i.e. weeks to months) often results in clinically meaningful improvements in HbA1c [19]. Of note, we previously found that structured exercise training sessions of as little as 30 min of aerobic, resistance or interval-type exercise result in lower TAR and increase TIR over the following 12–24 h compared with sedentary days [6], further supporting the health benefits of exercise training for those living with type 1 diabetes [3].
Short-term blood glucose responses to planned and unplanned physical activity are influenced by several factors in individuals with type 1 diabetes, including the time of day that activity is carried out, pre-exercise glucose levels, glucose rates of change before exercise, bolus insulin on board during activity and the activity type, duration and intensity [12]. In one notable study [5], the strategic use of short-duration moderate-intensity aerobic activities of varying time frames (<5 min, 5–10 min or 11–20 min) when glucose was elevated, resulted in improved TIR, without hypoglycaemia in youth with type 1 diabetes. Additionally, previous studies using the real-world T1DEXI dataset [6, 14] suggest that periods of structured exercise can improve short-term TIR in adults with type 1 diabetes by reducing TAR exposure, albeit with small increases in TBR. However, few studies have explored the relationship between daily step count, a proxy for planned and unplanned activity [8, 9], and CGM-based metrics in this population.
For within-participant analyses, we observed that days exceeding the step count goal (>10K) led to ~30 min more TIR but also ~5 min more TBR than days below the step count goal. Similarly, we observed lower mean glucose levels at day level when the step count goal was met (8.0±1.3 mmol/l) or exceeded (8.0±1.3 mmol/l) than when step count goals were not met (8.2±1.4 mmol/l; both p<0.001). These modest to weak associations between daily step count and TIR in the adult T1DEXI cohort agree with Drenthen et al [13], who observed an association between higher step counts and higher risks of hypoglycaemia in adults using MDI, as measured by blinded CGM and accelerometery. Furthermore, they are consistent with other research showing that increasing physical activity levels can increase TIR and reduce TAR, albeit accompanied by a slight increase in TBR [6, 20, 21]. The mean improvement in TIR on days when participants exceeded their step count goals compared with days below was 2.0%, which is considerably lower than the ~6% improvements previously seen using the T1DEXI dataset on days when participants completed a 30 min instructional exercise video session [6].
One possible explanation for this discrepancy could be that step count predominantly captures incidental walking, during which individuals with type 1 diabetes may not be as diligent in implementing pre- and post-exercise insulin adjustments, carbohydrate consumption and more vigilant glucose monitoring [22, 23]. Consequently, increasing daily (or hourly) step counts without concurrently implementing these strategies may yield different glycaemic benefits from a structured exercise regimen. Nonetheless, it is important to acknowledge that healthcare professionals and individuals with type 1 diabetes can still use step count as a marker of overall physical activity, which provides health benefits beyond TIR for this population.
Our within-participant analysis also demonstrated that high step count days (>10K) were associated with more risk for clinically significant level 2 hypoglycaemia. Specifically, 23% of participants had >1.0% of time with glucose <3.0 mmol/l (deemed as clinically concerning) on high (>10K) step count days compared with 18% of participants on lower (<10K) step counts days. Across the entire data collection period, three individuals developed level 3 hypoglycaemia overnight, all requiring assistance from another individual, two on days when the step count goals were met (7–10K) and one when they were exceeded (>10K). While these individuals did not attribute their episodes to increased activity per se, we suspect that higher than normal activity may have played some role.
When examining CGM-based metrics across all insulin modalities, regardless of step count group, HCL users demonstrated a higher TIR than MDI and standard insulin pump users. A lower TBR for HCL users on high step count days compared with MDI and pump users also suggests a protective effect of HCL systems on reducing hypoglycaemia risk relative to non-automated insulin-delivery tools. These differences may be partially attributable to the HCL system’s ability to automatically reduce insulin delivery in response to a drop in glucose concentration (or perhaps a higher temporary target in some activity events), with the intention of keeping users in a pre-determined safe glucose range (5.0–10.0 mmol/l) [24,25,26]. In line with this, less insulin delivery overnight, between 22:00 and 02:00, in HCL users compared with standard insulin pump users (0.81±1.09 U/h vs 0.98±0.33 U/h, respectively; p=0.008) has been reported in 12 individuals with type 1 diabetes (ages 12–26 years) following 1 h of brisk walking on a treadmill [25]. In our analyses, total daily insulin dose was significantly lower with increasing step count categories for standard insulin pump and HCL users, but not for MDI users (Table 4). This may suggest that pump users are more likely to self-impose insulin dose reductions on active days than those on MDI. As such, personalised insulin and carbohydrate feeding strategies may be needed, along with step count tracking and/or assessment, for individuals with type 1 diabetes on MDI who do not appear to change insulin delivery on more physically active days.
Irrespective of insulin modality, our analysis revealed that individuals with an elevated baseline HbA1c (≥53 mmol/mol [≥7.0%]) experienced improvements in mean glucose, TIR and TAR when they met or exceeded the step count goal compared with days below the goal. TBR was elevated only on days exceeding step count goals. The effects of step count on individuals with a baseline HbA1c <53 mmol/mol (<7.0%) were negligible; however, these findings suggest that achieving the step count goal (7–10K) may be optimal for improving TIR without posing an additional risk of hypoglycaemia, particularly for those with an elevated HbA1c.
The strengths of this study include its large cohort, month-long observation period and continuous assessment of daily step counts (blinded) and glucose metrics using a wrist-worn device and CGM. When worn during all waking hours for an extended period (e.g. 3–7 days), step count captured by wearable watches is a frequently used and validated objective measure of planned and unplanned physical activity [15]. Additionally, our analyses stratified individuals by three insulin-delivery modalities and according to mean daily step count (month level) and individual step counts (day level).
One limitation of the study is the cohort used. Participants had to be willing to try and meet the goal of 150 min of activity per week (inclusive of study exercise video sessions) and to use a Dexcom G6 continuous glucose monitor, suggesting that the cohort was likely to have been relatively active prior to participation, which would be reflected in insulin and carbohydrate feeding routines being titrated to this increased activity. Moreover, ~70% of the cohort used a standard insulin pump or HCL system, had a mean HbA1c of 48.8 mmol/mol (6.6%) and a mean TIR of 75%, which may not be representative of European or North American [27] adult type 1 diabetes populations. In addition, this study did not account for variations in step count due to other factors, such as activities with low or no step count (i.e. cycling, swimming, intensive short-term activity bouts), illness, stress or weekdays vs weekends. The method used for quantifying daily physical activity levels does not detail activity intensity, which may be more influential for interstitial glucose levels than total step count. Lastly, this study used CGM to determine TIR metrics, which is less accurate during times of rapid glucose changes, such as during exercise [28]. However, previous findings and limitations of the current study highlight the complexity of factors influencing the relationships between daily step count and glycaemic metrics in individuals with type 1 diabetes.
In conclusion, this study provides valuable insights into the relationship between daily step count and CGM-based metrics and glucose management in adults with type 1 diabetes. The results suggest that meeting the universally recommended guideline of 7–10K steps/day may lead to small reductions in TAR and marginal increases in TIR and TBR for adults living with type 1 diabetes. Future research should explore strategies to minimise hypoglycaemia risk in the active type 1 diabetes population, considering various insulin-delivery modalities and personalised management approaches.
Abbreviations
- 7000–10,000:
-
7–10K
- bpm:
-
Beats per minute
- CGM:
-
Continuous glucose monitoring
- HCL:
-
Hybrid closed-loop
- MDI:
-
Multiple daily insulin injections
- TAR:
-
Time above range (>10.0 mmol/l)
- TBR:
-
Time below range (<3.9 mmol/l)
- TIR:
-
Time in range (3.9–10.0 mmol/l)
References
Colberg SR, Laan R, Dassau E, Kerr D (2015) Physical activity and type 1 diabetes. J Diabetes Sci Technol 9(3):609–618. https://doi.org/10.1177/1932296814566231
Riddell MC, Pooni R, Fontana FY, Scott SN (2019) Diabetes technology and exercise. Endocrinol Metab Clin North Am 49(1):109–125. https://doi.org/10.1016/j.ecl.2019.10.011
Riddell MC, Peters AL (2023) Exercise in adults with type 1 diabetes mellitus. Nat Rev Endocrinol 19(2):98–111. https://doi.org/10.1038/s41574-022-00756-6
Diabetes Canada Clinical Practice Guidelines Expert Committee, Sigal RJ, Armstrong MJ et al (2018) Physical activity and diabetes. Can J Diabetes 42:S54–S63. https://doi.org/10.1016/j.jcjd.2017.10.008
Pemberton JS, Gupta A, Lau GM, Dickinson I, Iyer PV, Uday S (2023) Integrating physical activity strategies to lower hyperglycaemia in structured education programmes for children and young people with type 1 diabetes improves glycaemic control without augmenting the risk of hypoglycaemia. Pediatr Diabetes 2023:1–8. https://doi.org/10.1155/2023/2519368
Riddell MC, Li Z, Beck RW et al (2021) More time in glucose range during exercise days than sedentary days in adults living with type 1 diabetes. Diabetes Technol Ther 23(5):376–383. https://doi.org/10.1089/dia.2020.0495
Piercy KL, Troiano RP, Ballard RM et al (2018) The physical activity guidelines for americans. JAMA 320(19):2020–2028. https://doi.org/10.1001/jama.2018.14854
Kraus WE, Janz KF, Powell KE et al (2019) Daily step counts for measuring physical activity exposure and its relation to health. Medicine Sci Sports Exerc 51(6):1206–1212. https://doi.org/10.1249/mss.0000000000001932
Garber CE, Blissmer B, Deschenes MR et al (2011) American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Medicine Sci Sports Exerc 43(7):1334–1359. https://doi.org/10.1249/mss.0b013e318213fefb
del Pozo-Cruz J, Alvarez-Barbosa F, Gallardo-Gomez D, del Pozo Cruz B (2022) Optimal number of steps per day to prevent all-cause mortality in people with prediabetes and diabetes. Diabetes Care 45(9):2156–2158. https://doi.org/10.2337/dc22-0524
Anderson J, Couper JJ, Mpundu-Kaambwa C et al (2016) An extra 1,000 steps per day relates to improved cardiovascular health in children with type 1 diabetes. Diabetes Care 39(8):e108–e109. https://doi.org/10.2337/dc16-0526
Colberg SR, Sigal RJ, Yardley JE et al (2016) Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care 39(11):2065–2079. https://doi.org/10.2337/dc16-1728
Drenthen LCA, Ajie M, Bakker EA et al (2023) Daily unstructured physical activity affects mean glucose, occurrence of hypoglycaemia and glucose variability in people with type 1 diabetes. Diabetes Obes Metab 25(12):3837–3840. https://doi.org/10.1111/dom.15277
Riddell MC, Li Z, Gal RL et al (2023) Examining the acute glycemic effects of different types of structured exercise sessions in type 1 diabetes in a real-world setting: the Type 1 Diabetes and Exercise Initiative (T1DEXI). Diabetes Care 46(4):704–713. https://doi.org/10.2337/dc22-1721
Bassett DR, Toth LP, LaMunion SR, Crouter SE (2017) Step counting: a review of measurement considerations and health-related applications. Sports Med 47(7):1303–1315. https://doi.org/10.1007/s40279-016-0663-1
Battelino T, Danne T, Bergenstal RM et al (2019) Clinical targets for continuous glucose monitoring data interpretation: recommendations from the International Consensus on Time in Range. Diabetes Care 42(8):1593–1603. https://doi.org/10.2337/dci19-0028
Bohn B, Herbst A, Pfeifer M et al (2015) Impact of physical activity on glycemic control and prevalence of cardiovascular risk factors in adults with type 1 diabetes: a cross-sectional multicenter study of 18,028 patients. Diabetes Care 38(8):1536–1543. https://doi.org/10.2337/dc15-0030
Tikkanen-Dolenc H, Wadén J, Forsblom C et al (2017) Physical activity reduces risk of premature mortality in patients with type 1 diabetes with and without kidney disease. Diabetes Care 40(12):1727–1732. https://doi.org/10.2337/dc17-0615
Wu N, Bredin SSD, Guan Y et al (2019) Cardiovascular health benefits of exercise training in persons living with type 1 diabetes: a systematic review and meta-analysis. J Clin Med 8(2):253. https://doi.org/10.3390/jcm8020253
Adamo M, Codella R, Casiraghi F et al (2016) Active subjects with autoimmune type 1 diabetes have better metabolic profiles than sedentary controls. Cell Transplant 26(1):23–32. https://doi.org/10.3727/096368916x693022
Tonoli C, Heyman E, Roelands B et al (2012) Effects of different types of acute and chronic (training) exercise on glycaemic control in type 1 diabetes mellitus. Sports Med 42(12):1059–1080. https://doi.org/10.1007/bf03262312
McGaugh SM, Zaharieva DP, Pooni R et al (2021) Carbohydrate requirements for prolonged, fasted exercise with and without basal rate reductions in adults with type 1 diabetes on continuous subcutaneous insulin infusion. Diabetes Care 44(2):610–613. https://doi.org/10.2337/dc20-1554
Moser O, Eckstein ML, Mueller A et al (2019) Pre-exercise blood glucose levels determine the amount of orally administered carbohydrates during physical exercise in individuals with type 1 diabetes—a randomized cross-over trial. Nutrients 11(6):1287. https://doi.org/10.3390/nu11061287
Zaharieva DP, Messer LH, Paldus B, O’Neal DN, Maahs DM, Riddell MC (2020) Glucose control during physical activity and exercise using closed loop technology in adults and adolescents with type 1 diabetes. Can J Diabetes 44(8):740–749. https://doi.org/10.1016/j.jcjd.2020.06.003
Sherr JL, Cengiz E, Palerm CC et al (2013) Reduced hypoglycemia and increased time in target using closed-loop insulin delivery during nights with or without antecedent afternoon exercise in type 1 diabetes. Diabetes Care 36(10):2909–2914. https://doi.org/10.2337/dc13-0010
Dovc K, Macedoni M, Bratina N et al (2017) Closed-loop glucose control in young people with type 1 diabetes during and after unannounced physical activity: a randomised controlled crossover trial. Diabetologia 60(11):2157–2167. https://doi.org/10.1007/s00125-017-4395-z
Foster NC, Beck RW, Miller KM et al (2019) State of type 1 diabetes management and outcomes from the T1D Exchange in 2016–2018. Diabetes Technol Ther 21(2):66–72. https://doi.org/10.1089/dia.2018.0384
Moser O, Riddell MC, Eckstein ML et al (2020) Glucose management for exercise using continuous glucose monitoring (CGM) and intermittently scanned CGM (isCGM) systems in type 1 diabetes: position statement of the European Association for the Study of Diabetes (EASD) and of the International Society for Pediatric and Adolescent Diabetes (ISPAD) endorsed by JDRF and supported by the American Diabetes Association (ADA). Diabetologia 63(12):2501–2520. https://doi.org/10.1007/s00125-020-05263-9
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Acknowledgements
We would like to thank the T1DEXI study participants for taking the time to participate in this study.
Data availability
The data that support the findings reported here are available on the Vivli Platform Repository (ID: T1-DEXI; dataset name: Type 1 Diabetes EXercise Initiative (T1DEXI): The Effect of Exercise on Glycemic Control in Type 1 Diabetes Study; https://doi.org/https://doi.org/10.25934/PR00008428). The data package can be requested at https://doi.org/https://doi.org/10.25934/PR00008428.1.
Funding
This study was supported by The Leona M. and Harry B. Helmsley Charitable Trust. Verily (South San Francisco, CA) provided the Study Watch at no cost. Dexcom provided continuous glucose monitors at a discounted rate. CKM’s institution (Pennington Biomedical Research Center) is supported by a NORC Center grant (P30 DK072476) entitled ‘Nutrition and Metabolic Health Through the Lifespan’, sponsored by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), and by grant U54 GM104940 from the National Institute of General Medical Sciences, which funds the Louisiana Clinical and Translational Science Center. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Leona M. and Harry B. Helmsley Charitable Trust.
Authors’ relationships and activities
PGJ reports receiving grants from the National Institutes of Health, The Leona M. and Harry B. Charitable Trust, JDRF, Dexcom and the Oregon Health and Science University Foundation and consultancy fees from the Clinical Data Interchange Standards Consortium (CDISC); US patents 62/352,939, 63/269,094, 62/944,287, 8810388, 9,480,418, 8,317,700, 61/570382, 8,810,388, 7,976,466 and 6,558,321; and stock options from Pacific Diabetes Technologies, outside the submitted work. MAC is Chief Medical Officer of Glooko and has received grants or contracts from Dexcom, Abbott Diabetes Care, the National Institutes of Health, JDRF, the Emily Rosebud Foundation, Eli Lilly, Tolerion and Garmin. SRP reports receiving grants from The Leona M. and Harry B. Helmsley Charitable Trust, the National Institutes of Health and the Jaeb Center for Health Research, and honorarium from the ADA, outside the submitted work. JRC reports receiving grants from JDRF, the National Institutes of Health, Dexcom and Medtronic, and consultancy fees from Novo Nordisk, Insulet and Zealand, outside the submitted work. RWB reports receiving consulting fees, paid to his institution, from Insulet, Bigfoot Biomedical, vTv Therapeutics and Eli Lilly; grant support and supplies, provided to his institution, from Tandem and Dexcom; and supplies from Ascensia and Roche. MRR reports consultancy fees from Zealand Pharma. MCR reports receiving consulting fees from the Jaeb Center for Health Research, Eli Lilly, Zealand Pharma and Zucara Therapeutics; speaker fees from Sanofi Diabetes, Eli Lilly, Dexcom Canada and Novo Nordisk; and stock options from Supersapiens and Zucara Therapeutics. LVT, MCM, RLG, PC, ZL, CKM, FJD and MBG declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Contribution statement
RLG, PGJ, MAC, CKM, FJD, SRP, JRC, MBG, MRR and MCR contributed to the conception or design of the T1DEXI study. RLG, PGJ and MAC contributed to the acquisition of data. LVT, MCM, PC and ZL contributed to the data analysis. LVT, MCM, RLG, PC, ZL, RWB, MRR and MCR contributed to interpretation of the data. LVT and MCR drafted the manuscript. All authors reviewed the work critically for important intellectual content and approved the final version submitted for publication. MCR is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Turner, L.V., Marak, M.C., Gal, R.L. et al. Associations between daily step count classifications and continuous glucose monitoring metrics in adults with type 1 diabetes: analysis of the Type 1 Diabetes Exercise Initiative (T1DEXI) cohort. Diabetologia 67, 1009–1022 (2024). https://doi.org/10.1007/s00125-024-06127-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-024-06127-2