Abstract
Hematological malignancies may require rapid-onset treatment because of their short doubling time, notably observed in acute leukemias and specific high-grade lymphomas. Furthermore, in targeted onco-hematological scenarios, chemotherapy is deemed necessary as an emergency measure when facing short-term, life-threatening complications associated with highly chemosensitive hematological malignancies. The risks inherent in the disease itself, or in the initiation of treatment, may then require admission to the intensive care unit (ICU) to optimize monitoring and initial management protocols. Hyperleukocytosis and leukostasis in acute leukemias, tumor lysis syndrome, and disseminated intravascular coagulation are the most frequent onco-hematological complications requiring the implementation of emergency chemotherapy in the ICU. Chemotherapy must also be started urgently in secondary hemophagocytic lymphohistiocytosis. Tumor-induced microangiopathic hemolytic anemia and plasma hyperviscosity due to malignant monoclonal gammopathy represent infrequent yet substantial indications for emergency chemotherapy. In all cases, the administration of emergency chemotherapy in the ICU requires close collaboration between intensivists and hematology specialists. In this review, we provide valuable insights that aid in the identification and treatment of patients requiring emergency chemotherapy in the ICU, offering diagnostic tools and guidance for their overall initial management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In targeted onco-hematological scenarios, chemotherapy is deemed necessary as an emergency measure when facing short-term, life-threatening complications associated with highly chemosensitive hematological malignancies. |
The administration of emergency chemotherapy in the intensive care unit requires close collaboration between intensivists and hematology specialists, and may contribute to improving the prognosis of hematological malignancies. |
Introduction
Some hematological malignancies have short tumor doubling times (TDT) and specific related complications incompatible with scheduled initiation of treatment, necessitating rapid-onset chemotherapy. This emergency is particularly evident in highly chemosensitive diseases like acute leukemias and high-grade lymphomas, characterized by short TDT, initial chemosensitivity, and frequent life-threatening complications without prompt treatment [1,2,3].
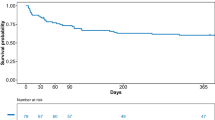
Chemotherapy administration in the intensive care unit (ICU) for malignancy-related complications, once considered a double-edged sword, has emerged as a potentially lifesaving intervention, even in the presence of concurrent infections or organ failures [2, 4, 5]. While studies focusing on ICU chemotherapy in hematological patients report mortality rates ranging from 25% [6] to 32% [2], available data suggest encouraging long-term outcomes with a reported 12-month survival rate of 30% among cancer patients receiving ICU chemotherapy, with 70% achieving complete remission [1].
Beyond drug-related toxicities, chemotherapy can exacerbate tumor-associated complications, potentially leading to life-threatening conditions. Hence, the initiation of chemotherapy represents a precarious phase that may necessitate preemptive ICU admission for optimized monitoring and management [7].
The literature on this topic is limited, and the beneficial effects of chemotherapy administered during ICU stays remain a subject of debate [8]. However, anticancer therapy in the ICU is feasible and might serve as a bridge to cure for selected, well-informed hematological patients with reasonable prognostic expectations [6, 9]. Intensivists play a crucial role in identifying patients who could benefit from urgent chemotherapy, collaborating closely with hematologists, as timely diagnostic and therapeutic interventions may significantly impact prognosis [4, 10].
In this review, we will first discuss common scenarios requiring or complicating urgent chemotherapy, most of the time in an ICU setting: hyperleukocytosis and leukostasis in acute leukemia, tumor lysis syndrome (TLS), and disseminated intravascular coagulation (DIC). Chemotherapy must also be started urgently in secondary hemophagocytic lymphohistiocytosis (HLH) [11]. Although less frequent, tumor-induced microangiopathic hemolytic anemia (MAHA) and plasma hyperviscosity due to malignant monoclonal gammopathy also necessitate prompt initiation of chemotherapy.
The objective of this review is to offer clinicians guidance and support in identifying and managing patients requiring urgent chemotherapy.
Hematological complications requiring emergency chemotherapy in the ICU
Hyperleukocytosis and leukostasis in acute leukemia
Hyperleukocytosis is often an unexpected finding in outpatients or in the emergency ward, frequently accompanied by non-specific symptoms like fever, dyspnea, or mucocutaneous bleeding. Hyperleukocytosis is defined as a circulating white blood cell count greater than 100 × 109/L [12], although the associated complications can occur as early as 50 × 109/L and may require ICU management. Hyperleukocytosis is present at diagnosis in up to 20% and 30% of patients with acute myeloid leukemia (AML) and with acute lymphoblastic leukemia (ALL) [13], respectively. Hyperleukocytosis can also be found in chronic leukemias, but is less commonly associated with complications, except in the acceleration phase of chronic myeloid or myelomonocytic leukemia, which highlights the role of circulating myeloid blasts in the genesis of leukostasis [14].
Leukostasis is a hyperviscosity syndrome involving cellular components encountered in up to 30% of hyperleukocytic AML [15], especially with monocytic characteristics and FLT3-ITD mutation [16]. Leukostasis is more rarely described in ALL, mostly in pediatric populations, and is associated with particularly high leukocytosis, greater than 400 × 109/L [14]. In this context, leukostasis often manifests alongside multiorgan failure, tumor lysis syndrome, and severe coagulopathy.
The pathophysiology of leukostasis involves endothelial dysfunction, due to the adhesion of blast cells to the endothelium, followed by their massive migration across the endothelial barrier [17]. This phenomenon is initiated by the exaggerated expression of integrins and selectins by leukemia cells, which amplify endothelial dysfunction through the production of proinflammatory cytokines [18]. The endothelial dysfunction leads to a rupture of the vascular barrier, a perivascular tissue infiltration by the blasts, and hemorrhagic phenomena. The role of hyperleukocytosis-induced blood hyperviscosity itself has long been suggested [19], and although it is only part of the mechanisms involved in leukostasis, this hyperviscosity underscores the importance of minimizing red blood cell transfusions during the hyperleukocytic phase of acute leukemia [14].
Pulmonary involvement is the most common manifestation of leukostasis, occurring in up to 40% of cases [20]. Clinical signs are non-specific and may include cough, dyspnea, and hypoxemia. Chest radiographs show non-specific patterns, with frequent bilateral diffuse alveolar infiltrates [21]. Pulmonary leukostasis often requires the initiation of mechanical ventilation as it can evolve into acute respiratory distress syndrome [22].
Brain involvement occurs in up to 30% of patients with leukostasis and manifests as delirium, focal neurologic deficits, or seizures. Brain imaging shows ischemic or hemorrhagic lesions that may be localized or diffuse [23], and in which blood hyperviscosity appears to play an important role (Fig. 1).
Inaugural complications of acute myeloid leukemia requiring emergency chemotherapy. A Pulmonary leukostasis, with bilateral alveolar and interstitial opacities, related to hyperleukocytic (230 × 109/L) acute monocytic leukemia (ex FAB-M5) at the time of diagnosis. B Pulmonary leukostasis, with ground-glass opacity in the right upper lobe, secondary to hyperleukocytic (200 × 109/L) acute myelomonocytic leukemia (ex FAB-M4). C Fundus image with fluorescein angiography revealing hyperviscosity-related retinopathy with disseminated retinal hemorrhages and vascular dilation. D, E T2*-weighted and T2-flair MRI sequences revealing inaugural left fronto-temporal hemorrhage and cerebral edema linked to hyperleukocytic (330 × 109/L) acute monocytic leukemia (ex FAB-M5). F Acute monocytic leukemia (ex FAB-M5): peripheral blood smear with numerous promonocytes that have folded and convoluted nuclei and a finely granulated cytoplasm and vacuoles. DIC disseminated intravascular coagulation, FAB French–American–British classification, MRI magnetic resonance imaging
Hyperleukocytosis, whether accompanied by leukostasis or not, is linked to a high mortality rate ranging from 25% to 50% in the initial weeks [17], which justifies ICU admission for close monitoring. Patients with hyperleukocytosis are at high-risk of respiratory deterioration after the initiation of induction chemotherapy, commonly termed acute lysis pneumopathy [22]. Effective management encompasses addressing organ failures and implementing treatments such as hyperhydration and urgent cytoreduction before introducing anthracycline and cytarabine-based induction chemotherapy (Table 1) [12].
Hydroxyurea has long been described as a reliable method to reduce cell counts, taper clinical leukostasis manifestations, and lower the risk of developing complications from the cytotoxic effects associated with definitive induction chemotherapy [24, 25]. The gradual reduction of cell counts with hydroxyurea has been shown to decrease hospital mortality in patients with hyperleukocytic AML when compared to a matched population that received induction chemotherapy without prior cytoreduction [24]. However, response to hydroxyurea has not been shown to be predictive of favorable short- and long-term outcomes [25]. The use of hydroxyurea is recommended by international guidelines to reduce white blood cells (WBC) count below 25 × 109/L although high-quality evidence to support this treatment is currently lacking [26].
Leukapheresis remains the frontline treatment for hyperleukocytosis and leukostasis in a large number of specialized centers worldwide [27]. While this procedure rapidly removes circulating blasts, it cannot eliminate cellular plugs already formed within vessels or inhibit cellular proliferation in the bone marrow. Although supported by several single-center retrospective studies [28], the largest study conducted to date found no discernible impact of leukapheresis on overall survival [15]. Additionally, the complications associated with central catheter insertion in patients with thrombocytopenia or DIC and the risk of catheter-related infection must be carefully considered before initiating leukapheresis. Various cytoreduction regimens have been described with no prospective data supporting the use of one strategy over another [29].
Alongside cytoreduction, the use of dexamethasone during induction chemotherapy has been suggested to reduce short-term mortality when compared with either a historical cohort or a propensity score-matched cohort that did not receive dexamethasone [30, 31]. No impact on infection occurrence has been demonstrated; however, there is a lack of prospective data supporting this claim. Dexamethasone has been shown to downregulate the expression of adhesion molecules involved in leucocytes adhesion, potentially alleviating the symptoms of leukostasis [32].
Tumor lysis syndrome
TLS is a life-threatening condition secondary to the release of tumor cells content into the bloodstream [33], including deoxyribonucleic acid (DNA) and its metabolites, intracellular ions (potassium, phosphorus), as well as evocative proteins like lactate dehydrogenase (LDH) and certain cytokines. The degradation of the purine bases of DNA (adenine, guanine) leads to the increase of plasmatic uric acid and the formation of uric acid crystals. Released phosphorus precipitates with calcium, which induces both hypocalcemia and the formation of calcium phosphate crystals [33, 34]. Thus, TLS-associated laboratory abnormalities include hyperuricemia, hyperphosphatemia, hypocalcemia, and hyperkalemia, which collectively define the biological TLS according to Cairo and Bishop (see supplementary Table 1). The combination of biological TLS with acute kidney injury (AKI), seizures (related to hypocalcemia), ventricular arrhythmia, or sudden cardiac death (related to hyperkalemia) defines the clinical TLS [35].
TLS arises in patients with chemosensitive malignancy and high tumor burden. It is therefore common in hyperleukocytic leukemia [17] or high-grade non-Hodgkin lymphomas such as Burkitt's lymphoma [36]. Although TLS mainly affects patients undergoing chemotherapy, spontaneous TLS might also occur. It is estimated that up to 40% of TLS happen spontaneously in high-risk patients [37]. Paradoxically, as a marker of high tumor burden, spontaneous TLS is an indication for urgent chemotherapy and close monitoring.
AKI severely affects the prognosis of TLS, and is associated with a 66% mortality rate at 6 months, compared to 21% in the absence of renal failure [37]. Thus, hyperhydration (3L/m2/day or 70 mL/kg) is the treatment’s cornerstone [33]. Alkalinization is no longer recommended because it is associated with the risk of precipitation of calcium phosphate crystals [38]. After stopping any phosphorus and potassium supplementation, the hydro-electrolyte rebalancing is aimed at correcting hyperkalemia by using polystyrene sulfonate alone in the absence of electrocardiographic (ECG) signs, and by combining insulin-glucose in hyperkalemia with ECG signs to avoid alkalinization. The efficacy of phosphate binders on hyperphosphatemia is disputed in this context, and hypocalcemia should not be supplemented (except in cases of convulsions, or hyperkalemia with ventricular arrhythmia) due to the precipitation of calcium with phosphorus [33]. Electrolyte disturbances (hyperkalemia, hyperphosphatemia) require initial monitoring in the ICU, including ECG monitoring.
Due to the risk of uratic nephropathy, the treatment includes a hypouricemic therapy, favoring rasburicase over allopurinol starting from the biological TLS stage [39]. However, ruling out glucose-6-phosphate dehydrogenase (G6PD) deficiency is essential beforehand to prevent rasburicase-induced methemoglobinemia.
Renal replacement therapy (RRT) should be discussed early [40], in addition to the usual criteria, in the event of persistent hyperphosphatemia, although no threshold could be determined by consensus [34]. In this context, the early consideration of hyperphosphatemia is part of an approach to prevent the onset or worsening of AKI. Clinical, ECG, and biological monitoring is essential before and during the initiation of anti-tumor treatment (cytoreduction or chemotherapy). The main biological abnormalities (serum potassium, phosphoremia, calcemia, uremia, creatinine, uric acid level, and eventually LDH) must be checked every 4–6 h during the acute phase [33].
Disseminated intravascular coagulation
DIC of tumor origin is encountered in different clinical forms depending on the causative malignancy, and is categorized into two groups: hyperfibrinolytic, associated with a hemorrhagic presentation, and antifibrinolytic, characterized by thrombotic manifestations [41]. The hemorrhagic phenotype is prominent in DIC induced by hematological malignancies and mainly concerns AML, while myeloproliferative disorders and asparaginase-treated ALL are preferentially associated with thrombotic phenotypes [41, 42].
Incidence of DIC among acute leukemias is estimated at 15–25% at the time of diagnosis [42]. The incidence is higher in the presence of hyperleukocytosis with leukostasis, especially in cases of AML that display a normal karyotype with FLT3-ITD mutation [43]. The pathophysiology of leukemia-induced DIC involves the production of tissue factor by leukemic cells, which triggers the coagulation cascade through the extrinsic pathway, and initiates multifactorial endothelial activation and dysfunction [44]. The hyperfibrinolytic and hemorrhagic presentation is particularly common in acute promyelocytic leukemia (APL), in which leukemia cells activate plasminogen through the expression of tissue plasminogen activator (tPA) thereby exacerbating fibrinolysis [45]. DIC is initially present in up to 80% of APL cases [42] according to the International Society on Thrombosis and Hemostasis (ISTH) definition [46]. ISTH criteria include thrombocytopenia, prolonged prothrombin time (PT), decreased fibrinogen, and increased fibrin degradation products (FDPs), or D-dimers. Thrombocytopenia is a questionable criterion in this context, as it may result from bone marrow invasion. Hence, the Japanese Ministry of Health and Welfare (JMHW) has proposed a platelet-free score for the diagnosis of DIC in patients with hematological malignancies (Table 2) [47].
Severe clinical manifestations of DIC are represented by cerebral hemorrhages, followed by intra-alveolar hemorrhages [42]. In patients with active bleeding, the platelet transfusion threshold should attain 50 × 109/L and fibrinogen replacement therapy is indicated to reach a level > 1.5 g/L [42, 48]. Acute leukemia-associated DIC is an indication for emergency cytoreduction and chemotherapy (Table 1). The treatment of DIC specifically induced by APL includes trans-retinoic acid (ATRA), which should be administered as soon as the diagnosis is established. However, ATRA can cause a differentiation syndrome in which the massive transformation of blasts into mature cells induces acute febrile multiorgan failure and whose treatment is based on dexamethasone and cytoreduction by hydroxyurea [49]. Importantly, with the advent of targeted therapies for AML, such as inhibitors targeting isocitrate dehydrogenase (IDH-1/2) and FMS-like tyrosine kinase 3 (FLT3), differentiation syndrome is now increasingly reported in non-APL AML [50]. Thrombotic manifestations are more often encountered in ALL, mostly secondary to the prothrombotic effect of l-asparaginase [51]. Through reduced concentrations of asparagine, hepatic synthesis of antithrombin and fibrinogen is lowered, resulting in both a prothrombotic state and hypofibrinogenemia in asparaginase-treated ALL patients [42]. Thus, antithrombin concentrates are recommended by the ISTH to achieve a target level of 80% to 120% and low-molecular-weight heparin thromboprophylaxis is strongly suggested in patients with a platelet count greater than 30 × 109/L without bleeding [51]. A lower threshold for platelet transfusion should be considered in asparaginase-treated ALL patients, but no precise guidelines have been published yet. Fibrinogen substitution is implemented in most studies to achieve a target level > 0.5 g/L [51]. Unfractionated heparin or low-molecular-weight heparin is used preferentially to oral anticoagulants to treat thromboembolic events [52].
Tumor-induced microangiopathic hemolytic anemia
Tumor-induced MAHA is a differential diagnosis of paraneoplastic DIC in the presence of peripheral thrombocytopenia [53]. In approximately 10–15% of cases, MAHA and DIC can co-exist [53, 54], and they appear to constitute the two facets of tumor-induced endothelial activation and dysfunction [41]. While DIC firstly activates secondary hemostasis through the production of tissue factor by endothelial cells, the pathophysiology of MAHA relies primarily on excessive platelet adhesion and activation, in correlation with an enhanced von Willebrand factor (VWF) activity of endothelial origin. Overexpression of VWF often accompanies a partial decrease in a disintegrin and metalloprotease with thrombospondin type I repeats-13 (ADAMTS13) protease activity [55], the physiological role of which is to cleave and inhibit VWF. This process leads to the formation of microthrombi, resulting in thrombocytopenia by consumption, and secondarily to intravascular hemolysis with the presence of schistocytes, by fragmentation of red blood cells in contact with microthrombi. Erythrocyte fragmentation may also be related to disseminated microvascular metastases or widespread bone marrow involvement [54, 56]. Therefore, the diagnosis of MAHA is based on a triad of thrombocytopenia, LDH elevation and the presence of schistocytes, along with a negative direct antiglobulin test. The search for schistocytes is a major diagnostic element and should be repeated in case of initial negativity [57].
Most cases of paraneoplastic MAHA occur in patients with solid tumors, followed in frequency by non-Hodgkin lymphomas [56, 58]. A notable characteristic of paraneoplastic MAHA is the prevalence of unclassified forms because they do not fit with hemolytic uremic syndrome (HUS) or thrombotic thrombocytopenic purpura (TTP) [58]. When available, ADAMTS13 activity is often decreased in tumor-induced MAHA, but does not reach the diagnostic threshold characterizing TTP (less than 10%), whether in solid tumors [59] or hematological malignancies [60]. This reinforces the idea that treatment strategies cannot be modeled on those used for TTP [61]. Corticosteroids, rituximab and caplacizumab cannot be universally recommended and should be considered on a case-by-case basis. In scenarios of suspected TTP without determined etiology, failure of plasmapheresis should raise the diagnosis of paraneoplastic MAHA, and in these circumstances bone marrow biopsy is recommended by some authors [56]. In the absence of recent clinical trials focused on paraneoplastic MAHA, only emergency chemotherapy has been shown to be associated with survival thus far [58]. Infectious or treatment-related etiologies must be ruled out, including gemcitabine, proteosome inhibitors (especially carfilzomib) and oxaliplatin therapy [54, 62]. Regarding immunomodulatory drugs, lenalidomide and checkpoint inhibitors may also trigger authentic immune-mediated TTP through the expression of an anti-ADAMTS 13 autoantibody [54]. Finally, hematopoietic stem cell transplantation (HSCT)-induced MAHA is a well-documented complication [54, 62]
Secondary hemophagocytic lymphohistiocytosis
Malignancy-associated secondary HLH is a hyperinflammatory state occurring in cancer patients. It results from an excessive stimulation of macrophages under the effect of an inappropriate cytokine production, especially interferon-ɣ by CD8+ T cells, accompanied by a loss of regulation by natural killer (NK) cells. Activated macrophages in turn produce cytokines in inappropriate quantities, including interleukin (IL) -6 and tumor necrosis factor (TNF), which is enhanced during cell lysis and boosted by tumor-infiltrating lymphocytes [11, 63]. Clinical signs are non-specific and include high fever, lymphadenopathy, and hepatosplenomegaly [11]. The hallmark biological signs combine cytopenia, hepatic cytolysis, hyperferritinemia, hypertriglyceridemia, and coagulation disorders, with hypofibrinogenemia being associated with mortality [63]. Hemophagocytosis, although frequently found in bone marrow aspiration smears, is not imperative for diagnosis. The diagnosis is based on the HLH-2004 diagnostic criteria (supplementary Table 2) [64]. The HScore (HLH-probability calculator) is an alternative diagnostic tool available online (http://saintantoine.aphp.fr/score/) [65]. Therefore, HLH is highly suspected if 5 of 8 criteria are fulfilled, and the diagnosis of HLH should be consistent with the overall clinical assessment and patient’s history [66]. Onco-hematological diseases account for 97% of malignancy-induced HLH, with non-Hodgkin lymphoma ranking first (roughly 74% of cases) followed by leukemia [11]. Secondary HLH is independently associated with mortality in lymphoma patients.
As untreated secondary HLH is systematically lethal [63], the administration of high-dose dexamethasone and emergency etoposide-based chemotherapy to eliminate activated T cells is a therapeutic priority in onco-hematological patients [66, 67]. Completion of the entire first-line chemotherapy regimen appropriate to the lymphoma subtype significantly improves patient prognosis. This includes combinations of rituximab, cyclophosphamide, doxorubicin, and vincristine in case of diffuse large B cell lymphoma (DLBCL) [68], resulting in an adapted regimen such as CHOEP (cyclophosphamide, doxorubicin, vincristine, etoposide, and prednisone) regimen [66].
Etoposide must also be administered urgently in certain non-malignant underlying indications, especially in the case of Epstein-Barr virus (EBV)-induced HLH, which requires the rapid addition of rituximab to deplete EBV-infected B-cells [11]. However, first-line administration of emergency chemotherapy does not apply to all cases of secondary HLH. For this reason, the etiological assessment of HLH must be meticulous, with the main treatment remaining that of the underlying cause. Ruxolitinib, a selective Janus kinase (JAK) inhibitor, used as a cytokine-reducing therapy with minimal myelosuppressive effects, is currently being incorporated into different treatment regimens for HLH secondary to hematological malignancies and HSCT. Emapalumab, a monoclonal antibody targeting interferon-gamma, is increasingly used in various centers for the treatment of secondary HLH. However, its application derived from a narrow subset of pediatric patients with primary HLH, warrants further assessment [69]. These new etoposide-reducing protocols help limit treatment toxicities before the initiation of disease-specific chemotherapy [70].
Plasma hyperviscosity
In contrast to “cellular” hyperviscosity, plasma hyperviscosity syndrome (HVS) results from an abnormal protein increase, often arising from plasma cell disorders with immunoglobulin (Ig). Due to their pentameric structure and their high molecular weight, IgMs are more likely to induce HVS, which explains the importance of Waldenström macroglobulinemia (WM) among etiologies [71, 72]. At diagnosis, 40% of WM patients present with HVS, compared to 3.4% of multiple myeloma (MM) patients [72, 73]. Notably, the presence of a cryoglobulin can trigger or worsen plasma hyperviscosity, due to the cold-induced polymerization of the immunoglobulin involved.
Clinical signs of plasma hyperviscosity are dominated by a triad [74], associating neurological abnormalities (headache, delirium, tinnitus, ataxia), visual disturbances (blurring, phosphenes, myodesopsia), and mucosal bleeding (epistaxis, gum). In a context of HVS suspicion or for asymptomatic patients with a high protein concentration, the diagnosis can be rapidly confirmed by ophthalmologic examination revealing delayed venule clearance and/or retinal hemorrhage [72, 73, 75]. Beyond major hyperproteinemia, serum protein electrophoresis reveals the monoclonal hypergammaglobulinemia, characterized by immunofixation, with levels of IgM, IgG, and IgA generally greater than 30, 40, and 60 g/L, respectively [71]. Cryoglobulinemia should be specifically screened, especially in the presence of IgM [76].
Main vital complications include thrombosis, digestive and cerebral bleedings. Thus, HVS represents a therapeutic emergency that should not be delayed for ophthalmic examination in symptomatic patients. Early management combines ICU admission, hyperhydration, and the elimination of all factors that may increase hyperviscosity, such as diuretics or red blood cell transfusions, except in case of active uncontrolled bleeding. Plasmapheresis, performed urgently at 40 mL/kg with albumin as the primary replacement fluid, except in cases of active hemorrhage, is essential [77]. One to three therapeutic plasma exchange(s) may be sufficient to resolve symptoms of HVS. In otherwise asymptomatic patients, retinal changes respond dramatically to a single TPE with marked or complete reversal of the fundoscopic findings [75].
As serum Ig levels will return to baseline in 4 weeks, etiological treatment should be initiated soon after plasma therapy, to avoid treatment clearance. For newly diagnosed WM with bulky disease, a combination of bendamustine and rituximab is recommended as first line therapy. Therapeutic alternatives include the dexamethasone–rituximab–cyclophosphamide combination in cases of low disease burden, as well as novel agents such as proteasome (bortezomib and carfilzomib) and Bruton's tyrosine kinase (BTK) inhibitors (ibrutinib) [72, 78]. The specific treatment of MM is detailed in the following paragraph.
Myeloma-associated complications
Beyond HVS, newly diagnosed or refractory MM typically presents with life-threatening complications such as hypercalcemia and AKI that may require ICU admission [79]. Light-chain cast nephropathy (LCCN) is the main cause of reversible AKI in MM patients and a frequent mode of diagnosis. LCCN must be evoked by the combination of low urinary albumin excretion and high free light chains (FLCs) level (> 500 mg/l) [79]. Renal recovery, which is a major predictive factor for survival, mostly depends on early reduction of serum FLCs, particularly in patients requiring RRT [80]. Therefore, specific treatment initiation is an emergency that should not be delayed by RRT and/or ICU admission [79].
Early management of MM-associated AKI is based on the combination of symptomatic measures and emergency chemotherapy with high-dose corticosteroids. By reducing the urinary concentration of FLCs and enhancing renal tubular flow, hyperhydration using saline fluids reduces the risk of intratubular precipitation [79]. The effectiveness of urine alkalinization remains controversial and should be avoided in hypercalcemic patients because of the risk of calcium phosphate precipitation [81].
Treatment of hypercalcemia relies on rehydration and intravenous bisphosphonates, adapted to estimated glomerular filtration rate (eGFR) value. While zoledronic acid is not contraindicated, pamidronate is preferred due to its lower risk of renal toxicity [82]. Despite controversial clinical benefit, calcitonin might be initiated concurrently, as bisphosphonates may require several days to exert their optimal therapeutic effects. Nephrotoxic treatments should be discontinued.
Due to its anti-inflammatory, cytotoxic, and catabolic properties, high-dose dexamethasone (40 mg/day) improves renal recovery [83] and should be administered immediately after the diagnosis [84]. Prudent hydration and reduced-dose (20 mg/day) dexamethasone might be considered in most frail patients (cardiovascular comorbidities, age > 80 years).
Initiating early anti-plasma cell chemotherapy is essential to reduce the tumor burden and monoclonal FLCs secretion. Currently, the standard of care in LCCN patients combines high-dose dexamethasone with the proteasome inhibitor bortezomib, whose efficacy and tolerance are established without dose adaptation, even in patients requiring RRT [83]. However, the broader use of lenalidomide, carfilzomib, or cyclophosphamide is constrained due to unfavorable toxicity profiles and limited renal metabolism within the LCCN setting [83, 85]. It is anticipated that in the coming years, the combination of bortezomib with the monoclonal anti-CD38 antibody daratumumab is likely to further improve both hematologic response and renal recovery [86].
In addition, extracorporeal removal of circulating FLCs through plasmapheresis or intensive hemodialysis using new-generation “high-cutoff” (HCO) protein–leaking dialyzers might be considered. This approach aims to prevent the persistent accumulation of FLCs in both vascular and extravascular compartments [80].
Conclusion
Indications for emergency chemotherapy are relatively rare, yet demand early recognition due to the potentially rapid and lethal nature presented of some malignant complications. Admission to the ICU must be considered for the implementation of emergency chemotherapy and overall initial management particularly when an initial worsening is expected, due to the disease itself and/or its treatment. Depending on the etiology, the rapid onset of the antineoplastic treatment may lead to complete recovery, justifying full-code management, especially in the case of initial treatment. The broadening of indications for ICU admission, requiring close interprofessional collaboration, may contribute to the major prognostic improvement reported in onco-hematological patients. Dedicated multicenter studies are warranted to assess both the efficacy and safety of emergency chemotherapies in the ICU.
References
Wohlfarth P, Staudinger T, Sperr WR, Bojic A, Robak O, Hermann A, Laczika K, Carlstrom A, Riss K, Rabitsch W, Bojic M, Knoebl P, Locker GJ, Obiditsch M, Fuhrmann V, Schellongowski P, Arbeitsgruppe fur hamato-onkologische Intensivmedizin der Osterreichischen Gesellschaft fur Internistische und Allgemeine Intensivmedizin und N (2014) Prognostic factors, long-term survival, and outcome of cancer patients receiving chemotherapy in the intensive care unit. Ann Hematol 93:1629–1636
Benoit DD, Depuydt PO, Vandewoude KH, Offner FC, Boterberg T, De Cock CA, Noens LA, Janssens AM, Decruyenaere JM (2006) Outcome in severely ill patients with hematological malignancies who received intravenous chemotherapy in the intensive care unit. Intensive Care Med 32:93–99
Song JU, Suh GY, Chung MP, Kim H, Kwon OJ, Jung CW, Kang WK, Park K, Jeon K (2011) Risk factors to predict outcome in critically ill cancer patients receiving chemotherapy in the intensive care unit. Support Care Cancer 19:491–495
Moors I, Pene F, Lengline E, Benoit D (2015) Urgent chemotherapy in hematological patients in the ICU. Curr Opin Crit Care 21:559–568
Vandijck DM, Benoit DD, Depuydt PO, Offner FC, Blot SI, Van Tilborgh AK, Nollet J, Steel E, Noens LA, Decruyenaere JM (2008) Impact of recent intravenous chemotherapy on outcome in severe sepsis and septic shock patients with hematological malignancies. Intensive Care Med 34:847–855
Pastores SM, Goldman DA, Shaz DJ, Kostelecky N, Daley RJ, Peterson TJ, Tan KS, Halpern NA (2018) Characteristics and outcomes of patients with hematologic malignancies receiving chemotherapy in the intensive care unit. Cancer 124:3025–3036
Lengline E, Raffoux E, Lemiale V, Darmon M, Canet E, Boissel N, Schlemmer B, Dombret H, Azoulay E (2012) Intensive care unit management of patients with newly diagnosed acute myeloid leukemia with no organ failure. Leuk Lymphoma 53:1352–1359
de Oliveira MCF, Ferreira JC, Nassar Junior AP, Dettino ALA, Caruso P (2020) Impact of urgent chemotherapy in critically ill patients. J Intensive Care Med 35:347–353
Zerbib Y, Rabbat A, Fartoukh M, Bige N, Andrejak C, Mayaux J, De Prost N, Misset B, Lemiale V, Bruneel F, Maizel J, Ricome S, Jacobs F, Bornstain C, Dupont H, Baudin F, Azoulay E, Pene F, Groupe de Recherche sur la Reanimation Respiratoire en O-H (2017) Urgent chemotherapy for life-threatening complications related to solid neoplasms. Crit Care Med 45:e640–e648
Sekeres MA, Elson P, Kalaycio ME, Advani AS, Copelan EA, Faderl S, Kantarjian HM, Estey E (2009) Time from diagnosis to treatment initiation predicts survival in younger, but not older, acute myeloid leukemia patients. Blood 113:28–36
Vick EJ, Patel K, Prouet P, Martin MG (2017) Proliferation through activation: hemophagocytic lymphohistiocytosis in hematologic malignancy. Blood Adv 1:779–791
Dohner H, Weisdorf DJ, Bloomfield CD (2015) Acute myeloid leukemia. N Engl J Med 373:1136–1152
Desprez C, Kouatchet A, Marchand T, Mear JB, Tadie JM, Peterlin P, Chevalier P, Canet E, Couturier MA, Guillerm G, Bodenes L, Gyan E, Villate A, Ehrmann S, Lebreton A, Lester MA, Fronteau C, Larhantec G, Andre V, Riou J, Hunault-Berger M, Schmidt-Tanguy A, Orvain C (2023) Outcome of patients with newly diagnosed AML admitted to the ICU, including preemptive admission—a multi-center study. Ann Hematol 102:1383–1393
Macaron W, Sargsyan Z, Short NJ (2022) Hyperleukocytosis and leukostasis in acute and chronic leukemias. Leuk Lymphoma 63:1780–1791
Stahl M, Shallis RM, Wei W, Montesinos P, Lengline E, Neukirchen J, Bhatt VR, Sekeres MA, Fathi AT, Konig H, Luger S, Khan I, Roboz GJ, Cluzeau T, Martinez-Cuadron D, Raffoux E, Germing U, Umakanthan JM, Mukherjee S, Brunner AM, Miller A, McMahon CM, Ritchie EK, Rodriguez-Veiga R, Itzykson R, Boluda B, Rabian F, Tormo M, Acuna-Cruz E, Rabinovich E, Yoo B, Cano I, Podoltsev NA, Bewersdorf JP, Gore S, Zeidan AM (2020) Management of hyperleukocytosis and impact of leukapheresis among patients with acute myeloid leukemia (AML) on short- and long-term clinical outcomes: a large, retrospective, multicenter, international study. Leukemia 34:3149–3160
Thiede C, Steudel C, Mohr B, Schaich M, Schakel U, Platzbecker U, Wermke M, Bornhauser M, Ritter M, Neubauer A, Ehninger G, Illmer T (2002) Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: association with FAB subtypes and identification of subgroups with poor prognosis. Blood 99:4326–4335
Bewersdorf JP, Zeidan AM (2020) Hyperleukocytosis and leukostasis in acute myeloid leukemia: can a better understanding of the underlying molecular pathophysiology lead to novel treatments? Cells 9:2310
Stucki A, Rivier AS, Gikic M, Monai N, Schapira M, Spertini O (2001) Endothelial cell activation by myeloblasts: molecular mechanisms of leukostasis and leukemic cell dissemination. Blood 97:2121–2129
Steinberg MH, Charm SE (1971) Effect of high concentrations of leukocytes on whole blood viscosity. Blood 38:299–301
Porcu P, Danielson CF, Orazi A, Heerema NA, Gabig TG, McCarthy LJ (1997) Therapeutic leukapheresis in hyperleucocytic leukaemias: lack of correlation between degree of cytoreduction and early mortality rate. Br J Haematol 98:433–436
Stefanski M, Jamis-Dow C, Bayerl M, Desai RJ, Claxton DF, Van de Louw A (2016) Chest radiographic and CT findings in hyperleukocytic acute myeloid leukemia: a retrospective cohort study of 73 patients. Medicine (Baltimore) 95:e5285
Moreau AS, Lengline E, Seguin A, Lemiale V, Canet E, Raffoux E, Schlemmer B, Azoulay E (2014) Respiratory events at the earliest phase of acute myeloid leukemia. Leuk Lymphoma 55:2556–2563
Algharras AA, Mamourian A, Coyne T, Mohan S (2013) Leukostasis in an adult with AML presenting as multiple high attenuation brain masses on CT. J Clin Diagn Res 7:3020–3022
Mamez AC, Raffoux E, Chevret S, Lemiale V, Boissel N, Canet E, Schlemmer B, Dombret H, Azoulay E, Lengline E (2016) Pre-treatment with oral hydroxyurea prior to intensive chemotherapy improves early survival of patients with high hyperleukocytosis in acute myeloid leukemia. Leuk Lymphoma 57:2281–2288
Cerrano M, Seegers V, Raffoux E, Rabian F, Sebert M, Itzykson R, Lemiale V, Ades L, Boissel N, Dombret H, Azoulay E, Lengline E (2020) Predictors and outcomes associated with hydroxyurea sensitivity in acute myeloid leukemia patients with high hyperleukocytosis. Leuk Lymphoma 61:737–740
Dohner H, Wei AH, Appelbaum FR, Craddock C, DiNardo CD, Dombret H, Ebert BL, Fenaux P, Godley LA, Hasserjian RP, Larson RA, Levine RL, Miyazaki Y, Niederwieser D, Ossenkoppele G, Rollig C, Sierra J, Stein EM, Tallman MS, Tien HF, Wang J, Wierzbowska A, Lowenberg B (2022) Diagnosis and management of AML in adults: 2022 recommendations from an international expert panel on behalf of the ELN. Blood 140:1345–1377
Stahl M, Pine A, Hendrickson JE, Litzow MR, Luger SM, Stone RM, Erba HP, Kim TK, Sekeres MA, Steensma DP, Komrokji RS, Gore SD, Zeidan AM (2018) Beliefs and practice patterns in hyperleukocytosis management in acute myeloid leukemia: a large U.S. web-based survey(). Leuk Lymphoma 59:2723–2726
Ventura GJ, Hester JP, Smith TL, Keating MJ (1988) Acute myeloblastic leukemia with hyperleukocytosis: risk factors for early mortality in induction. Am J Hematol 27:34–37
Zhao J, Bewersdorf JP, Jaszczur S, Kowalski A, Perreault S, Schiffer M, Gore S, Podoltsev N, Prebet T, Shallis R, Zeidan AM (2021) High dose cyclophosphamide for cytoreduction in patients with acute myeloid leukemia with hyperleukocytosis or leukostasis. Leuk Lymphoma 62:1195–1202
Azoulay E, Canet E, Raffoux E, Lengline E, Lemiale V, Vincent F, de Labarthe A, Seguin A, Boissel N, Dombret H, Schlemmer B (2012) Dexamethasone in patients with acute lung injury from acute monocytic leukaemia. Eur Respir J 39:648–653
Cerrano M, Chevret S, Raffoux E, Rabian F, Sebert M, Valade S, Itzykson R, Lemiale V, Ades L, Boissel N, Dombret H, Azoulay E, Lengline E (2023) Benefits of dexamethasone on early outcomes in patients with acute myeloid leukemia with hyperleukocytosis: a propensity score matched analysis. Ann Hematol 102:761–768
Nakagawa M, Bondy GP, Waisman D, Minshall D, Hogg JC, van Eeden SF (1999) The effect of glucocorticoids on the expression of L-selectin on polymorphonuclear leukocyte. Blood 93:2730–2737
Howard SC, Jones DP, Pui CH (2011) The tumor lysis syndrome. N Engl J Med 364:1844–1854
Zafrani L, Canet E, Darmon M (2019) Understanding tumor lysis syndrome. Intensive Care Med 45:1608–1611
Cairo MS, Bishop M (2004) Tumour lysis syndrome: new therapeutic strategies and classification. Br J Haematol 127:3–11
Darmon M, Vincent F, Camous L, Canet E, Bonmati C, Braun T, Caillot D, Cornillon J, Dimicoli S, Etienne A, Galicier L, Garnier A, Girault S, Hunault-Berger M, Marolleau JP, Moreau P, Raffoux E, Recher C, Thiebaud A, Thieblemont C, Azoulay E, Groupe de Recherche en Reanimation Respiratoire et O-H (2013) Tumour lysis syndrome and acute kidney injury in high-risk haematology patients in the rasburicase era. A prospective multicentre study from the Groupe de Recherche en Reanimation Respiratoire et Onco-Hematologique. Br J Haematol 162:489–497
Darmon M, Guichard I, Vincent F, Schlemmer B, Azoulay E (2010) Prognostic significance of acute renal injury in acute tumor lysis syndrome. Leuk Lymphoma 51:221–227
Jones GL, Will A, Jackson GH, Webb NJ, Rule S, Committee B, for Standards in H, (2015) Guidelines for the management of tumour lysis syndrome in adults and children with haematological malignancies on behalf of the British Committee for Standards in Haematology. Br J Haematol 169:661–671
Alakel N, Middeke JM, Schetelig J, Bornhauser M (2017) Prevention and treatment of tumor lysis syndrome, and the efficacy and role of rasburicase. Onco Targets Ther 10:597–605
Matuszkiewicz-Rowinska J, Malyszko J (2020) Prevention and treatment of tumor lysis syndrome in the era of onco-nephrology progress. Kidney Blood Press Res 45:645–660
Helms J, Iba T, Connors JM, Gando S, Levi M, Meziani F, Levy JH (2023) How to manage coagulopathies in critically ill patients. Intensive Care Med 49:273–290
Wang TF, Makar RS, Antic D, Levy JH, Douketis JD, Connors JM, Carrier M, Zwicker JI (2020) Management of hemostatic complications in acute leukemia: guidance from the SSC of the ISTH. J Thromb Haemost 18:3174–3183
Guo Z, Chen X, Tan Y, Xu Z, Xu L (2020) Coagulopathy in cytogenetically and molecularly distinct acute leukemias at diagnosis: comprehensive study. Blood Cells Mol Dis 81:102393
Ten Cate H, Leader A (2021) Management of disseminated intravascular coagulation in acute leukemias. Hamostaseologie 41:120–126
Kwaan HC, Weiss I, Tallman MS (2019) The role of abnormal hemostasis and fibrinolysis in morbidity and mortality of acute promyelocytic leukemia. Semin Thromb Hemost 45:612–621
Taylor FB Jr, Toh CH, Hoots WK, Wada H, Levi M, Scientific Subcommittee on Disseminated Intravascular Coagulation of the International Society on T, Haemostasis (2001) Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost 86:1327–1330
Yanada M, Matsushita T, Suzuki M, Kiyoi H, Yamamoto K, Kinoshita T, Kojima T, Saito H, Naoe T (2006) Disseminated intravascular coagulation in acute leukemia: clinical and laboratory features at presentation. Eur J Haematol 77:282–287
Squizzato A, Hunt BJ, Kinasewitz GT, Wada H, Ten Cate H, Thachil J, Levi M, Vicente V, D’Angelo A, Di Nisio M (2016) Supportive management strategies for disseminated intravascular coagulation. An international consensus. Thromb Haemost 115:896–904
Sanz MA, Fenaux P, Tallman MS, Estey EH, Lowenberg B, Naoe T, Lengfelder E, Dohner H, Burnett AK, Chen SJ, Mathews V, Iland H, Rego E, Kantarjian H, Ades L, Avvisati G, Montesinos P, Platzbecker U, Ravandi F, Russell NH, Lo-Coco F (2019) Management of acute promyelocytic leukemia: updated recommendations from an expert panel of the European LeukemiaNet. Blood 133:1630–1643
Norsworthy KJ, Mulkey F, Scott EC, Ward AF, Przepiorka D, Charlab R, Dorff SE, Deisseroth A, Kazandjian D, Sridhara R, Beaver JA, Farrell AT, de Claro RA, Pazdur R (2020) Differentiation syndrome with ivosidenib and enasidenib treatment in patients with relapsed or refractory IDH-mutated AML: a U.S. Food and Drug Administration systematic analysis. Clin Cancer Res 26:4280–4288
Orvain C, Balsat M, Tavernier E, Marolleau JP, Pabst T, Chevallier P, de Gunzburg N, Cacheux V, Huguet F, Chantepie S, Caillot D, Chalandon Y, Frayfer J, Bonmati C, Lheritier V, Ifrah N, Dombret H, Boissel N, Hunault-Berger M (2020) Thromboembolism prophylaxis in adult patients with acute lymphoblastic leukemia treated in the GRAALL-2005 study. Blood 136:328–338
Rank CU, Toft N, Tuckuviene R, Grell K, Nielsen OJ, Frandsen TL, Marquart HVH, Albertsen BK, Tedgard U, Hallbook H, Ruud E, Jarvis KB, Quist-Paulsen P, Huttunen P, Wartiovaara-Kautto U, Jonsson OG, Trakymiene SS, Griskevicius L, Saks K, Punab M, Schmiegelow K (2018) Thromboembolism in acute lymphoblastic leukemia: results of NOPHO ALL2008 protocol treatment in patients aged 1 to 45 years. Blood 131:2475–2484
Wada H, Matsumoto T, Suzuki K, Imai H, Katayama N, Iba T, Matsumoto M (2018) Differences and similarities between disseminated intravascular coagulation and thrombotic microangiopathy. Thromb J 16:14
Thomas MR, Scully M (2021) How I treat microangiopathic hemolytic anemia in patients with cancer. Blood 137:1310–1317
Colonne CK, Favaloro EJ, Pasalic L (2022) The intriguing connections between von Willebrand Factor, ADAMTS13 and cancer. Healthcare (Basel) 10(3):557
Decaestecker A, Hamroun A, Provot F, Rondeau E, Faguer S, Sallee M, Titeca-Beauport D, Rebibou JM, Forestier A, Azar R, Deltombe C, Wynckel A, Grange S, Fremeaux Bacchi V, Cartery C (2023) Retrospective study of 59 cases of cancer-associated thrombotic microangiopathy: presentation and treatment characteristics. Nephrol Dial Transplant 38:913–921
Schmidt J, Zafrani L, Lemiale V, Stepanian A, Joly B, Azoulay E, Mariotte E (2021) The clinical picture of thrombotic microangiopathy in patients older than 60 years of age. Br J Haematol 192:e25–e28
Lechner K, Obermeier HL (2012) Cancer-related microangiopathic hemolytic anemia: clinical and laboratory features in 168 reported cases. Medicine (Baltimore) 91:195–205
Fontana S, Gerritsen HE, Kremer Hovinga J, Furlan M, Lammle B (2001) Microangiopathic haemolytic anaemia in metastasizing malignant tumours is not associated with a severe deficiency of the von Willebrand factor-cleaving protease. Br J Haematol 113:100–102
Yui JC, Garceau D, Jhaveri KD, Wanchoo R, Bijol V, Glezerman I, Hassoun H, Dispenzieri A, Russell SJ, Leung N (2019) Monoclonal gammopathy-associated thrombotic microangiopathy. Am J Hematol 94:E250–E253
Azoulay E, Bauer PR, Mariotte E, Russell L, Knoebl P, Martin-Loeches I, Pene F, Puxty K, Povoa P, Barratt-Due A, Garnacho-Montero J, Wendon J, Munshi L, Benoit D, von Bergwelt-Baildon M, Maggiorini M, Coppo P, Cataland S, Veyradier A, Van de Louw A, Nine-i I (2019) Expert statement on the ICU management of patients with thrombotic thrombocytopenic purpura. Intensive Care Med 45:1518–1539
Valerio P, Barreto JP, Ferreira H, Chuva T, Paiva A, Costa JM (2021) Thrombotic microangiopathy in oncology—a review. Transl Oncol 14:101081
Valade S, Mariotte E, Azoulay E (2020) Coagulation disorders in hemophagocytic lymphohistiocytosis/macrophage activation syndrome. Crit Care Clin 36:415–426
Henter JI, Horne A, Arico M, Egeler RM, Filipovich AH, Imashuku S, Ladisch S, McClain K, Webb D, Winiarski J, Janka G (2007) HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer 48:124–131
Fardet L, Galicier L, Lambotte O, Marzac C, Aumont C, Chahwan D, Coppo P, Hejblum G (2014) Development and validation of the HScore, a score for the diagnosis of reactive hemophagocytic syndrome. Arthritis Rheumatol 66:2613–2620
La Rosee P, Horne A, Hines M, von Bahr GT, Machowicz R, Berliner N, Birndt S, Gil-Herrera J, Girschikofsky M, Jordan MB, Kumar A, van Laar JAM, Lachmann G, Nichols KE, Ramanan AV, Wang Y, Wang Z, Janka G, Henter JI (2019) Recommendations for the management of hemophagocytic lymphohistiocytosis in adults. Blood 133:2465–2477
Arca M, Fardet L, Galicier L, Riviere S, Marzac C, Aumont C, Lambotte O, Coppo P (2015) Prognostic factors of early death in a cohort of 162 adult haemophagocytic syndrome: impact of triggering disease and early treatment with etoposide. Br J Haematol 168:63–68
Li B, Guo J, Li T, Gu J, Zeng C, Xiao M, Zhang W, Li Q, Zhou J, Zhou X (2021) Clinical characteristics of hemophagocytic lymphohistiocytosis associated with non-Hodgkin B-cell lymphoma: a multicenter retrospective study. Clin Lymphoma Myeloma Leuk 21:e198–e205
Garonzi C, Chinello M, Cesaro S (2021) Emapalumab for adult and pediatric patients with hemophagocytic lymphohistiocytosis. Expert Rev Clin Pharmacol 14:527–534
Stalder G, Suffiotti M, Segot A, Noto A, Pantaleo G, Spertini O, Obeid M (2023) Response-adjusted regimen combining ruxolitinib, etoposide and dexamethasone (adRED) in adult patients with acute myeloid leukemia-associated hemophagocytic lymphohistiocytosis: a single-center pilot trial. Haematologica 108:234–239
Gustine JN, Meid K, Dubeau T, Hunter ZR, Xu L, Yang G, Ghobrial IM, Treon SP, Castillo JJ (2017) Serum IgM level as predictor of symptomatic hyperviscosity in patients with Waldenstrom macroglobulinaemia. Br J Haematol 177:717–725
Weaver A, Rubinstein S, Cornell RF (2020) Hyperviscosity syndrome in paraprotein secreting conditions including Waldenstrom macroglobulinemia. Front Oncol 10:815
Debureaux PE, Harel S, Parquet N, Lemiale V, Siguret V, Goubeau L, Morin F, Royer B, Cuccuini W, Elessa D, Theves F, Brignier AC, Azoulay E, Arnulf B, Talbot A (2022) Prognosis of hyperviscosity syndrome in newly diagnosed multiple myeloma in modern-era therapy: a real-life study. Front Immunol 13:1069360
Fahey JL, Barth WF, Solomon A (1965) Serum hyperviscosity syndrome. JAMA 192:464–467
Dumas G, Gabarre P, Bige N, Maury E (2018) Hyperviscosity syndrome. Intensive Care Med 44:1151–1152
Stone MJ (2009) Waldenstrom’s macroglobulinemia: hyperviscosity syndrome and cryoglobulinemia. Clin Lymphoma Myeloma 9:97–99
Bauer PR, Ostermann M, Russell L, Robba C, David S, Ferreyro BL, Cid J, Castro P, Juffermans NP, Montini L, Pirani T, Van De Louw A, Nielsen N, Wendon J, Brignier AC, Schetz M, Kielstein JT, Winters JL, Azoulay E, Nine II (2022) Plasma exchange in the intensive care unit: a narrative review. Intensive Care Med 48:1382–1396
Gertz MA (2017) Waldenstrom macroglobulinemia: 2017 update on diagnosis, risk stratification, and management. Am J Hematol 92:209–217
Bridoux F, Leung N, Belmouaz M, Royal V, Ronco P, Nasr SH, Fermand JP, International K, Monoclonal Gammopathy Research G (2021) Management of acute kidney injury in symptomatic multiple myeloma. Kidney Int 99:570–580
Hutchison CA, Cockwell P, Stringer S, Bradwell A, Cook M, Gertz MA, Dispenzieri A, Winters JL, Kumar S, Rajkumar SV, Kyle RA, Leung N (2011) Early reduction of serum-free light chains associates with renal recovery in myeloma kidney. J Am Soc Nephrol 22:1129–1136
Sathick IJ, Drosou ME, Leung N (2019) Myeloma light chain cast nephropathy, a review. J Nephrol 32:189–198
Perazella MA, Markowitz GS (2008) Bisphosphonate nephrotoxicity. Kidney Int 74:1385–1393
Bridoux F, Arnulf B, Karlin L, Blin N, Rabot N, Macro M, Audard V, Belhadj K, Pegourie B, Gobert P, Cornec Le Gall E, Joly B, Karras A, Jaccard A, Augeul-Meunier K, Manier S, Royer B, Caillot D, Tiab M, Delbes S, Suarez F, Vigneau C, Caillard S, Arakelyan-Laboure N, Roos-Weil D, Chevret S, Fermand JP (2020) Randomized trial comparing double versus triple bortezomib-based regimen in patients with multiple myeloma and acute kidney injury due to cast nephropathy. J Clin Oncol 38:2647–2657
Bayraktar UD, Warsch S, Pereira D (2011) High-dose glucocorticoids improve renal failure reversibility in patients with newly diagnosed multiple myeloma. Am J Hematol 86:224–227
Dimopoulos MA, Roussou M, Gavriatopoulou M, Psimenou E, Ziogas D, Eleutherakis-Papaiakovou E, Fotiou D, Migkou M, Kanellias N, Panagiotidis I, Ntalianis A, Papadopoulou E, Stamatelopoulos K, Manios E, Pamboukas C, Kontogiannis S, Terpos E, Kastritis E (2017) Cardiac and renal complications of carfilzomib in patients with multiple myeloma. Blood Adv 1:449–454
Peigne V, Rusinova K, Karlin L, Darmon M, Fermand JP, Schlemmer B, Azoulay E (2009) Continued survival gains in recent years among critically ill myeloma patients. Intensive Care Med 35:512–518
Acknowledgements
This work received non-financial support from the Grrr-OH Network (Groupe de Recherche en Réanimation Respiratoire du patient d’Onco-Hématologie) and CRICS group (Clinical Research in Intensive Care and Sepsis). We warmly thank Elie Azoulay (Saint Louis Hospital, Paris, France), who had the initial idea for writing this review, for his helpful contribution. We are also grateful to Guillaume Dumas (Grenoble, France) and Sofiane Fodil (Saint Louis Hospital, Paris, France) for authorization to use fundus and peripheral blood smear images.
Author information
Authors and Affiliations
Consortia
Contributions
All the authors participated in the writing and editing of the manuscripts. AL and RCJ reviewed the clinical trials.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no competing financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lafarge, A., Chean, D., Whiting, L. et al. Management of hematological patients requiring emergency chemotherapy in the intensive care unit. Intensive Care Med (2024). https://doi.org/10.1007/s00134-024-07454-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00134-024-07454-z